Topics

The VASRD is updated every now and then by the VA and Congress. Each change is meant to make the VASRD more fair and complete. Since it takes a very long time to get anything through the VA’s study groups and committees, the VASRD is not changed very often, and when it is, the changes are normally pretty small. There have, however, been some big changes in the past, and the VA is currently in the process of rewriting the entire VASRD, so more changes will be coming soon.
On this page, we discuss all the historic VASRDs from 2001 to the present and the major changes that were made with each update. Everything on this page is no longer in effect for the current ratings but still apply to all rating decisions made during the applicable time periods.
The changes are listed from newest (most recent) to oldest.
When we list a date, we describe what the historic VASRD was like BEFORE the change since each change brings the historic VASRDs closer to the current VASRD.
If a condition is not discussed below, then it means that it is exactly the same as the current VASRD, and you can simply Find Your Condition on this site.
Additionally, all the code numbers for each condition below is linked to the current version of that condition. Just click on the codes to go to the current ratings. If the code number is not linked to anything, it means that code no longer exists.
For example, on January 19, 2012 the VA changed the rating for Amyotrophic Lateral Sclerosis (ALS). Before this date, ALS was rated a minimum of 30%. After this date, it was the same as the current VASRD (100%—see our discussion of ALS). So, if you were rated ON or AFTER January 19, 2012, you’ll get the current rating for ALS. If you were rated BEFORE January 19, 2012, then your ALS is rated a minimum of 30%, which we discuss in detail below. Got it?
Again, we’ll give a date and then discuss the historic VASRD criteria that existed BEFORE that date. If you fall after that date, find the condition on our site. If you fall before that date, read on to see how it was rated.
IMPORTANT! There are a few conditions that have had their ratings changed more than once during the time period we are covering. Make sure you pay attention to this! For example, the ratings for the Skin changed THREE times: once in 2002, once in 2008, and again in 2018. If you were rated before the 2002 date, then check out the change for that date. If between the 2002 date and the 2008 date, check out the change for the 2008 date. If after the 2018 date, it is rated on the current VASRD for The Skin, etc.
November 14, 2021 – Genitourinary System
Code 7542: A Neurogenic Bladder occurs when a person loses control over urination because of damage to the nerves or the brain. This condition is rated on the Urinary Rating System.
Code 7545 for Diverticulum of the bladder did not exist before this date.
A urinary tract infection is a bacterial infection that can affect the upper urinary tract (these can be called a kidney infection) or the lower urinary tract (a bladder infection). These infections are normally treated and cured with no disability. However, if a condition results in multiple urinary tracts infections it can be rated based on the severity and frequency of the infections.
The ratings: A 30% rating is given if the condition causes regular infections that require hospitalization 3 or more times a year, or if it requires serious continuous treatment. A 10% rating is given if the condition requires regular drug therapy, 1 or 2 hospitalizations a year, or if it requires serious continuous treatment.
If any of these conditions that are rated as urinary tract infections also cause renal problems, then only one or the other can be rated. If the renal problems are more severe, then the condition should be rated under the renal rating system.
The following conditions are rated as urinary tract infections:
Code 7501: Abscess of the Kidney is a puss-filled pocket in the kidney.
Code 7525: Chronic Epididymo-orchitis is pain in the Epididymis. If the pain is caused by tuberculosis, it is rated as nonpulmonary tuberculosis.
Code 7527: Prostate Gland conditions (any) are either rated as urinary tract infections or by the urinary rating system, whichever better defines the symptoms of the condition.
A 100% rating is given if at least one of the following is present:
- The condition requires regular dialysis.
- The body cannot perform any physical activity because of persistent Edema or because of Albuminuria.
- A BUN of more than 80 mg/dL.
- A Creatinine level of 9 mg/dL or more in the blood.
- A severely decreased functioning of the kidneys or other organs due to kidney dysfunction.
An 80% rating is given if one or more of the following is present:
- Persistent Edema and Albuminuria with a BUN of 40 to 80 mg/dL.
- A Creatinine level of 4 to 8 mg/dL in the blood.
- Overall poor health with symptoms like lethargy, weakness, anorexia, weight loss, or the inability to exert much energy.
A 60% rating is given if one or more of the following is present:
- Constant Albuminuria with some Edema.
- A definite decrease in kidney function.
- Hypertension with the average diastolic pressure (the smaller number on the bottom in the blood pressure reading) of 120 or more.
A 30% rating is given if one or more of the following is present:
- Occasional or slight Edema.
- Hypertension with the average diastolic pressure (the smaller number on the bottom) of 100 or more, or with the average systolic pressure (the larger number on top) of 160 or more.
- Albumin is present in the urine with either Hyaline and Granular casts or red blood cells.
A 0% rating is given if:
- Hypertension with the average diastolic pressure of less than 100, or with the average systolic pressure of less than 160.
- Albumin and casts are present in the urine with a history of nephritis.
Code 7533: Any cystic disease of the kidney is rated under this code. A cyst is a sac most often containing fluid that can grow anywhere in the body. Many do not cause problems, but some can seriously affect the functioning of the organs.
Code 7534: Atherosclerotic renal disease (also known as renal artery stenosis or atheroembolic renal disease) is a condition where the artery to the kidney narrows and decreases the blood flow to the kidney.
Code 7537: Interstitial nephritis occurs when the spaces between the tubules in the kidney swell. This reduces the ability of the kidneys to filter blood.
Code 7539: Renal amyloid disease is caused by the buildup of protein in the kidney, which may result in the kidney not being able to filter blood.
Code 7541: Renal Involvement in other conditions. So, if the kidneys are affected by conditions like sickle cell anemia, lupus, or diabetes, it can be rated separately from those conditions.
Code 7544 for Renal disease caused by viral infections did not exist before this date.
Code 7508: Nephrolithiasis (also known as kidney stones) is the presence of stones in the kidney or Ureter. These stones block the flow of urine through the tubes. This condition is rated as hydronephrosis unless stones are repeatedly formed and it requires either drug therapy, diet therapy, or removal surgeries or procedures 3 or more times each year. If this is the case, it is rated 30%. Otherwise, rate as hydronephrosis.
Code 7510: Ureterolithiasis is the presence of stones in the Ureter. These stones can block the flow of urine through the tubes. This condition is rated as hydronephrosis unless stones are repeatedly formed and it requires either drug therapy, diet therapy, or removal surgeries or procedures 3 or more times each year. If this is the case, it is rated 30%. Otherwise, rate as hydronephrosis.
Code 7520: If half or more of the penis is removed, then it is rated 30%. This condition can also be rated under the urinary rating system if that can result in a higher rating than 30%.
Code 7521: If the Glans is removed, it is rated 20%. This condition can also be rated under the urinary rating system if that can result in a higher rating than 20%.
Code 7522: If the penis is deformed and cannot erect, then it is rated 20%.
Code 7543 for Varicocele and hydrocele did not exist before this date.
November 14, 2021 – Cardiovascular System
Basic Rating System for the Heart
The majority of heart conditions are rated based on a set rating system. All the conditions will be listed below along with any deviations from this rating system.
Note: It is very important that the physician performing your exam gets an MET (metabolic equivalent of task) test done for ANY heart condition. An MET test, more often known as an exercise test, checks for how much oxygen is being used by the body to perform increasingly strenuous tasks. 1 MET equals the amount of oxygen a person uses when at rest. There are a very few cases where an MET test is not required, but the majority of the time it is essential to getting a proper heart rating. Be proactive and make sure an MET test is done!
It is also vital that the need for medication for the condition and whether or not there is hypertrophy or dilation is clearly recorded by the physician.
The basic rating system:
A 100% rating is given if there is one or more of the following:
- Continuous congestive heart failure
- The condition scores 3 METs or less on an MET test and causes shortness of breath, fatigue, chest pain, dizziness or fainting
- Left ventricular dysfunction with an ejection fraction of less than 30%
A 60% rating is given if there is one or more of the following:
- Two or more episodes of congestive heart failure in the past year
- The condition scores 4 or 5 METs and causes shortness of breath, fatigue, chest pain, dizziness or fainting
- Left ventricular dysfunction with an ejection fraction between 30 and 50%
A 30% rating is given if there is one or more of the following:
- The condition scores 6 or 7 METs on an MET test and causes shortness of breath, fatigue, chest pain, dizziness or fainting
- Evidence (x-ray, electro-cardiogram, or echocardiogram) of hypertrophy or dilation. An electro-cardiogram by itself can prove hypertrophy, but is not enough to prove dilation.
A 10% rating is given if there is one or more of the following:
- The condition scores 8, 9 or 10 METs and causes shortness of breath, fatigue, chest pain, dizziness or fainting
- Continuous medication is required
All of the heart conditions in this section must be officially diagnosed using appropriate testing (echocardiogram, cardiac catheterization, etc.).
A 100% rating is given for the following conditions while the condition is active and continues for the first three months following the end of treatment or hospitalization for the condition. After that, the conditions are rated based on the basic rating system.
- Code 7000: Valvular heart disease includes any disease, including rheumatic heart disease, that involves one or more valves of the heart. Rheumatic heart disease usually develops many years after the initial infection which causes the condition. Because of this, it can be judged to have existed prior to service and thus is not ratable even if it was not diagnosed before entering the military. Medical findings of murmurs or valvular lesions early in your career could be enough to prove it did exist prior to service.
- Code 7001: Endocarditis is the inflammation of the lining of the heart chambers and valves.
- Code 7002: Pericarditis is the inflammation of the covering tissue surrounding the heart.
- Code 7006: Myocardial infarction (or a “heart attack”) occurs when the blood flow to a part of the heart is blocked, thus causing damage to the heart muscle. (For DoD purposes, a heart attack which occurs while on active duty will be considered as caused by service unless it is clearly proven to not be related).
- Code 7017: Coronary bypass surgery is performed if there is a block in a coronary artery. The surgeon grafts veins or arteries from the aorta directly to the artery, thus bypassing the block. The three-month period for this condition begins the day of admission to the hospital for the procedure.
The following conditions are given a 100% rating for an “indefinite” period of time before they are rated on the basic rating system.
- Code 7011: Sustained ventricular arrhythmias are abnormal heart rhythms, most commonly too fast, that are located in the heart’s two lower chambers. These rhythms can come and go and are usually treated with medication or electric therapy. This condition receives the 100% rating the entire time it is being treated in the hospital or the entire time an implantable defibrillator is in place. If a pacemaker is implanted, then it is rated under code 7018.
- Code 7016: A heart valve replacement is performed when a valve of the heart is not functioning properly. It is replaced by an artificial valve that can perform the function of the damaged valve. This receives the 100% rating the entire time it is being treated in the hospital and for 6 months following discharge from the hospital. At the 6-month mark, the condition is reevaluated. It then either continues with the 100% rating or is rated based on the basic rating system.
- Code 7018: Cardiac pacemakers are implanted if the rhythm of the heart is too slow. This condition is rated 100% for the first 2 months following the surgery. After that, it is rated under the base condition that caused the irregular heart rhythm: supraventricular arrhythmias, ventricular arrhythmias, or an atrioventricular block. The minimum rating for a condition requiring a pacemaker is 10%. If a defibrillator is implanted, then it is rated under code 7011.
- Code 7019: Cardiac transplantation, a heart transplant, is rated 100% for at least one year from the date of admission to the hospital. One year after discharge, the condition is re-evaluated and rated on the basic rating system. The minimum rating for this condition is 30%.
The following conditions do not have the 100% rating periods described for the above conditions. Instead, these are immediately rated on the basic rating system.
- Code 7003: Pericardial adhesions occur when the sac surrounding the heart sticks to the heart muscle and restricts its pumping action.
- Code 7004: Syphilitic heart disease occurs many years after the initial infection of syphilis. It causes inflammation in the heart that restricts blood flow to the heart itself. It can also cause syphilitic Aortic Aneurysms, but those should be rated under code 7110.
- Code 7005: Ischemic heart disease, Arteriosclerotic heart disease, Atherosclerotic heart disease, or Coronary artery disease all affect the coronary arteries. Arteriosclerosis is the thickening and hardening of the walls of the arteries, atherosclerosis is the narrowing and hardening of the arteries, and coronary artery disease is the blocking of the arteries from the build up of plaque. Often coronary artery disease is present with the other two. Coronary artery disease must be clearly documented to rate this condition.
- Code 7007: Hypertensive heart disease is caused by high blood pressure. Hypertension over many years can result in left ventricular hypertrophy and/or heart failure.
- Code 7015: Atrioventricular block occurs when the electrical impulses that allow the different parts of the heart to communicate and function are blocked. This must be associated with other evidence of heart disease to be considered unfitting. It is rated on the basic rating system with one addition: if a pacemaker is required, it is rated 10%.
- Code 7020: Cardiomyopathy is the deterioration of the heart muscle and its functioning for any reason. Any heart condition that is not covered by the other heart codes is rated here.
Other Heart Conditions:
Code 7009 for Bradycardia did not exist prior to this date.
Code 7010: Supraventricular arrhythmias are abnormal heart rhythms, most commonly too fast, that are located in the heart’s two upper chambers. If episodes of abnormal heart rhythms occur 5 or more times a year, then it is rated 30%. A 10% rating is given if episodes of abnormal rhythm occur 1 to 4 times a year or if there is permanent atrial fibrillation with no evidence of other heart diseases or conditions. All episodes must be properly documented by an ECG Test.
Artery and Vein Conditions
Code 7110: If an aneurysm in the aortic artery is corrected by surgery, then it is rated 100% from the day of admittance to the hospital. This rating continues for the first 6 months after discharge from the hospital. The condition is then reevaluated and rated accordingly. If the condition is active and causes symptoms such as pain or hemorrhaging, or if it is 5 centimeters or larger in diameter, then it is rated 100%. If the condition is serious enough that you cannot perform any activities requiring exertion (anything that increases heart rate), then it is rated 60%. If the condition does not qualify for these ratings, then it is rated based on the existing symptoms in the affected organ (e.g. if it caused erratic heart beats, then it would be rated as arrhythmia).
Code 7111: If an aneurysm in any large artery (except the aortic artery) is surgically corrected, then it is rated 100% from the date of admission to the hospital. This rating continues for the first 6 months after discharge from the hospital. The condition is then reevaluated and rated accordingly. A 100% rating is given if there is pain in the limbs (claudication) and either tears in the skin of the limbs from lack of oxygen or the Ankle Brachial Index is 0.4 or less.
A 60% rating is given if you cannot walk further than 25 yards without limping because of pain and one or more of the following: there is coldness in the limb that does not respond to warming methods, there are one or more tears in the skin of the limb, or the ankle brachial index is 0.5 or less.
A 40% rating is given if you have limping because of pain when walking between 25 and 100 yards and one or more of the following: there are 1.) changes to the hair, skin, or nails of the affected limb, or 2.) the ankle brachial index is 0.7 or less.
A 20% rating is given if you have limping because of pain when walking more than 100 yards and one or more of the following: the pulse in the limb is diminished, or the ankle brachial index is 0.9 or less.
Note: These ratings are for a single limb only. If more than one limb has an aneurysm, then rate each separately.
Code 7113: A traumatic arteriovenous fistula is an abnormal passageway between an artery and a vein. They are most often caused by penetrating wounds that affected nearby arteries or veins, thus causing the body to create a false passageway to continue blood flow. They can cause the heart to have to work harder to provide the necessary blood to all regions of the body, thus leading to various heart conditions. It can also cause loss of blood flow to the limbs resulting in pain, infection, swelling, skin changes, or amputation.
If the condition causes heart failure, then it is rated 100%. If the heart has not failed, but is enlarged with a rapid pulse and a Wide Pulse Pressure, then it is rated 60%. If the heart is not affected, but in an arm there is swelling, Stasis Dermatitis, and either tears in the skin or a cellulitis infection, then it is rated 40%. If a leg has swelling, stasis dermatitis, and either tears in the skin or a cellulitis infection, it is rated 50%. If there is only swelling or stasis dermatitis in a leg, then it is rated 30%. If the swelling or stasis dermatitis is in an arm, it is rated 20%.
Code 7114 and 7115 are rated on the same system.
Code 7114: Arteriosclerosis obliterans (a.k.a. peripheral vascular disease) is the thickening and hardening of the tissues of a vessel that causes the vessel to narrow and develop blood clots. This condition most often affects the aorta artery in the abdomen and the small or medium vessels in the legs.
Code 7115: Thrombo-angiitis obliterans (or “Buerger’s Disease”) is a disease where the blood vessels of the hands or feet become blocked due to the build up of plaque. It is mostly associated with the use of tobacco products. It causes pain and swelling in the hands and feet and could result in necessary amputation.
The ratings:
A 100% rating is given if there is pain in the limbs and either tears in the skin of the limbs from lack of oxygen or the Ankle Brachial Index is 0.4 or less.
A 60% rating is given if you cannot walk further than 25 yards without limping because of leg pain (claudication) and one or more of the following: there is coldness in the limb that does not respond to warming methods, there are one or more tears in the skin of the limb, or the ankle brachial index is 0.5 or less.
A 40% rating is given if there is limping because of leg pain when walking between 25 and 100 yards and one or more of the following: there are 1.) changes to the hair, skin, or nails of the affected limb, or 2.) the ankle brachial index is 0.7 or less.
A 20% rating is given if there is limping because of leg pain when walking more than 100 yards and one or more of the following: the pulse in the limb is diminished, or the ankle brachial index is 0.9 or less.
Note: The above ratings are for a single limb only. If more than one limb is affected, then rate each separately.
Code 7122: Frostbite and other conditions caused by overexposure to the cold can cause permanent damage to the arteries, nerves, and veins and are rated on the persistent symptoms of the condition.
A 30% rating is given if there is joint pain, numbness, or sensitivity to the cold in the area affected and two or more of the following: discoloration of the skin, abnormal nail growth, tissue loss, decreased ability to feel, Hyperhidrosis, or other abnormalities proven by x-ray.
A 20% rating is given if there is joint pain, numbness, or sensitivity to the cold in the area affected and one of the following: discoloration of the skin, abnormal nail growth, tissue loss, decreased ability to feel, hyperhidrosis, or other abnormalities proven by x-ray.
A 10% rating is given if there is only pain, numbness, or sensitivity to the cold in the affected area.
These ratings are for individual parts affected. So if a foot and a hand are both affected, then they each receive a separate rating. This does not include individual toes or fingers—if one or more fingers or toes are affected, then it is just rated once on the hand or foot.
Any other conditions resulting from overexposure to the cold not listed under this code are to be rated separately, including amputations, carcinomas and neuropathies.
Code 7124 for Raynaud’s Disease did not exist before this date.
February 7, 2021 – Musculoskeletal System and Muscle Injuries
Code 5002: Rheumatoid arthritis is the destruction of the soft tissues in a joint because of swelling.
Regardless of how many joints are affected, if the arthritis is severe enough that you cannot function, but are completely incapacitated and bedridden, then it is rated 100%.
If there is significant weight loss, anemia, and overall severe decrease in health but not complete incapacitation, or if severe incapacitating episodes happen 4 or more times a year, then it is rated 60%.
If there is a definite decline in overall health, or if incapacitating episodes happen 3 or more times a year, then it is rated 40%.
One or two episodes a year rates 20%.
These ratings cannot be used in addition to ratings for limited motion. One or the other. Any rheumatoid arthritis less severe than noted above is just rated upon its symptoms, such as limited motion. In these cases individual joints can be rated. So, if three joints are involved, but there are no incapacitating episodes, all three can be rated separately on limited motion. A minimum of 10% is given for every joint that at least has pain with motion.
Code 5009: All other arthritis is included under this code and rated as 5002, rheumatoid arthritis.
Code 5010: Post-traumatic arthritis is arthritis that is due to an accident or injury. This code doesn’t have its own ratings, but is rated as degenerative arthritis. The final code for this condition will look like this: 5010-5003. The first four-digit code defines the condition as traumatic arthritis, and the second four-digit code tells how it is rated.
Code 5011: Caisson disease is the premature death of bone and marrow cells, often caused by compressed air most often seen in divers. It is rated based on its most prevalent symptom. For example, if it affects the spinal cord and causes limited motion in the hip, it would be rated under that symptom. Common symptoms include deafness, arthritis in the joints, loss of motion, etc. Only the symptom that can give the highest rating can be rated for this condition. The final code for this condition would look like this: 5011-5261. The first four-digit code identifies the condition as caisson disease, and the second four-digit code tells what symptom the condition is rated under.
Code 5018: Intermittent hydrarthrosis is the periodic swelling most commonly of Major Joints, although other joints could also be affected, on a regular and predictable schedule. This code no longer exists.
Code 5020: Synovitis is the swelling of a membrane that lines Synovial Joints. This code no longer exists.
Code 5022: Periostitis is the swelling of the tissue that surrounds the bones. This code no longer exists.
Code 5024: Tenosynovitis is the swelling of the tissues that surround the tendons.
Code 5051: If the entire shoulder joint has been replaced by a prosthetic device, the condition is rated 100% for the first year after the surgery. (This period is mainly for the VA, but the DoD will also use it if the veteran is placed on TDRL before being permanently separated). After the 1-year period, the condition is given a permanent rating. If there is weakness and severe pain with motion, then it is rated 60% for the Dominant arm and 50% for the Non-dominant arm.
If there are occasional periods of weakness, pain or limited motion, then the condition should be rated analogously (see the Analogous and Equivalent Codes page) either under code 5002, rheumatoid arthritis, or 5203, impairment of the clavicle or scapula, whichever most closely describes the condition’s symptoms. The final code for these analogous ratings look like this: 5051-5002. The first four-digit code defines the condition as a shoulder replacement, and the second code tells how the condition is rated.
The minimum rating for any total shoulder replacement is 30% for the Dominant arm and 20% for the Non-dominant arm.
Note: This code is only for total shoulder replacements. Partial replacements are rated on any symptoms that they cause, like limited motion.
Code 5052: If the entire elbow joint has been replaced by a prosthesis, then the condition is rated 100% for the first year after the surgery. (This period is mainly for VA Disability, but DoD Disability will also use it if the veteran is placed on TDRL before being permanently separated). After the 1-year period, the condition is given a permanent rating. If there is weakness and/or severe pain with motion, then it is rated 50% for the Dominant arm and 40% for the Non-dominant. If the pain is not severe, but does limit the range of motion, then it is rated Analogously (see the Analogous and Equivalent Codes page) under code 5205, 5206, 5207, or 5208 whichever best fits the condition. The minimum rating for a total elbow replacement is 30% for the dominant arm and 20% for the non-dominant arm regardless of how much motion it has.
Note: This code is only for total elbow replacements. Partial replacements are rated on any symptoms that they cause, like limited motion.
Code 5053: If the entire wrist joint has been replaced by a prosthesis (false joint), then the condition is rated 100% for the first year after being discharged from the hospital following the surgery (this period is mainly for the VA, but the DoD may also give this 1-year rating if the veteran is placed on TDRL before being permanently separated).
After the 1-year period, the condition is given a permanent rating. If there is weakness and severe pain with motion, then it is rated 40% for the Dominant hand and 30% for the Non-dominant hand. If the pain is not severe, but does limit the range of motion, then it is rated under the code 5215, discussed below. The minimum rating for a total wrist replacement, however, is 20% for either hand regardless of how much motion it has.
Note: This code is only for total wrist replacements. Partial replacements are rated on any symptoms that they cause, like limited motion.
Code 5054: If either the entire head of the femur or entire head of the acetabulum has been replaced by a false joint prosthesis, then the condition is rated 100% for the first year after the surgery. (This period is mainly for the VA, but the DoD will also use it if the veteran is placed on TDRL before being permanently separated). After the 1-year period, the condition is given a permanent rating. If there is weakness and severe pain with motion that requires the use of crutches, then it is rated 90%. If there is weakness and severe pain, but it does not require crutches, then it is rated 70%. If the pain is not severe, but does limit the range of motion, then it is rated 50%. The minimum rating for a hip replacement is 30%.
If your condition rates 90% under this code, you may also qualify for additional compensation by the VA. Please see the Special Monthly Compensation page for more information.
Code 5055: If the entire knee joint has been replaced by a Prosthesis, then the condition is rated 100% for the first year after the surgery. (This period is mainly for the VA, but the DoD will also use it if the veteran is placed on TDRL before being permanently separated). After the 1-year period, the condition is given a permanent rating. If there is weakness and severe pain with motion, then it is rated 60%. If the pain is not severe, but does limit the range of motion, then it is rated under code 5256 if it is frozen, or under codes 5261 or 5262, discussed below, if it is not frozen. The minimum rating for a total knee replacement, however, is 30% regardless of how much motion it has.
Note: This code is only for total knee replacements. Partial replacements are rated on any symptoms that they cause, like limited motion.
Code 5056: If the entire ankle joint has been replaced by a false joint prosthesis, then the condition is rated 100% for the first year after the surgery. This 1-year period begins after the one month allowed under principle §4.30 after being discharged from the hospital (this principle is mainly for the VA, but the DoD may also abide by this principle if the veteran is placed on TDRL before being permanently separated).
After the 1-year period, the condition is given a permanent rating. If there is continual weakness or severe pain with motion, then it is rated 40%. If the pain and/or weakness are not continual or severe, but does limit the range of motion, then it is rated under the codes 5270 or 5271 discussed above. The minimum rating for a total ankle replacement, however, is 20% regardless of how much motion it has.
Note: This code is only for total ankle replacements. Partial replacements are rated on any symptoms that they cause, like limited motion.
Code 5120: If the entire arm is amputated from the shoulder joint down, it is rated 90% for either arm.
Code 5160: If the entire leg is amputated at the hip joint, it is rated 90%.
Code 5170: If all the toes are amputated, not including the ball of the foot, it is rated 30%.
Code 5242: Degenerative arthritis of the spine is first rated under the general rating formula. If this condition is not severe enough to be rated on that formula, then it is rated as degenerative arthritis, code 5003.
Code 5244 for paraplegia and quadriplegia did not exist before this date.
Code 5255: Any problems with the femur or femoral neck bones are rated under this code. If either is completely broken through and it causes loose or erratic leg motion, then it is rated 80%. If it is broken through but the leg motion is not loose and the leg can support weight with the help of a brace, then it is rated 60%. If it is fractured and has a false joint, it is rated 60%.
All other femur bone conditions are rated by how they affect the hip or knee joint. If they cause serious problems (can barely use the joint at all), then it is a 30% rating. If the joints can be used, but the condition significantly limits the amount of activity, then it is rated 20%. If the hip or knee joint is affected only slightly, then it is rated 10%.
Code 5257: The knee can also have too much motion (instability) from side to side or dislocate regularly. This can happen when the tendons and cartilage are damaged and can no longer support the knee joint properly. If there is only Slight Instability, then it is rated 10%. If there is more instability that might cause the knee to buckle or dislocate every now and then, then it is rated 20%. If, however, it is so unstable that it gives out or dislocates regularly, it is rated 30%.
Code 5262: Any problems with the tibia or fibula bones in the lower leg are rated under this code. If there is a complete break in either bone that cannot heal and requires a brace, then it is rated 40%. All other conditions are rated by how they affect the knee or ankle joint. If they cause serious problems (can barely use the joint at all), then it is a 30% rating. If the joints can be used, but the condition significantly limits the amount of activity, then it is rated 20%. If the knee or ankle joint is affected only slightly, then it is rated 10%.
Code 5271: If the ankle is not frozen, but limited in motion, then it is rated under this code. Normal range of motion for the ankle is 0° to 20° dorsiflexion and 0° to 45° plantar flexion. A 20% rating is given for a markedly limited range of motion and a 10% is given for a moderately limited range of motion.
Code 5269: Plantar fasciitis did not exist before this date.
Code 5330: Rhabdomyolysis did not exist before this date.
Code 5331: Compartment Syndrome did not exist before this date.
August 11, 2019 – Infectious Diseases and Immune Disorders
The General Rating System for Infectious Diseases did not exist before this date.
Code 6300: Asiatic cholera is an infection in the small intestine that causes severe diarrhea and vomiting. The 100% rating for this condition continues for 3 months after the active infection. If there are symptoms left over after the 3-month period, then they are rated separately. These symptoms could include Papillary Necrosis, which is rated under code 7538.
Code 6301: Visceral leishmaniasis is a disease of parasites in the internal organs that can cause symptoms like weight loss, fever, and anemia. The 100% rating for this condition continues for the first 6 months after treatment for this disease ends. It is then reevaluated, and any remaining symptoms or side effects are rated separately. These symptoms could include liver damage, which is rated under code 7312.
Code 6302: Leprosy (or “Hansen’s Disease”) is a bacterial disease that attacks the skin, nerves and airways. It causes severe skin damage and can lead to many other conditions if left untreated. The 100% rating for this condition continues for the first 6 months after treatment for this disease ends. It is then reevaluated, and any remaining symptoms or side effects are rated separately. These symptoms could include skin damage, codes 7800–7805, or nerve damage. Nerve damage is a bit complicated to rate, and the code depends on which nerves are damaged. Thorough information on rating nerve damage can be found on The Central Nervous System page.
Code 6304: Malaria is a disease of parasites that infect red blood cells and cause severe fevers and other symptoms. For malaria to be properly diagnosed, it must be confirmed by blood smear tests unless it is clear that the veteran was in an area where contamination could be very likely. The 100% rating for this condition continues only while the condition is active. Afterwards, any remaining side effects are rated separately. These symptoms could include liver damage, which is rated under code 7312.
Code 6305: Lymphatic filariasis is a disease of parasites that infect the lymphatic system, including the Lymph Nodes. The 100% rating for this condition continues only while the condition is active. Afterwards, any remaining symptoms or side effects are rated separately. These symptoms could include Epididymitis, which is rated under code 7525.
Code 6306: Bartonellosis is a bacterial infection which can cause many other diseases including trench fever, chronic bacteremia, endocarditis, neurological conditions, Carrion’s disease, cat-scratch disease, bacillary angiomatosis, peliosis hepatis, and chronic lymphadenopathy. All of these conditions are rated under this code. The 100% rating for this condition continues only while the condition is active. Afterwards, any remaining symptoms or side effects are rated separately. These symptoms could include skin damage, which is rated under codes 7800–7805.
Code 6307: Plague (any kind) is a bacterial infection that can attack different parts of the body. It can be treated if caught early. The 100% rating for this condition continues only while the condition is active. After that, any remaining side effects or symptoms are rated separately. These symptoms could include Gangrene that could lead to amputation. It would then be rated on the amputation of the particular body part. See the Amputations page for a complete list of amputation ratings. In addition to gangrene, this condition could also cause nerve or brain damage. The code depends on the extent of the nerve or brain damage. All nerve and brain conditions are discussed on The Central Nervous System page.
Code 6308: Relapsing fever is a bacterial infection that causes fevers, chills, aches, and nausea that can last between 2 and 9 days. Every couple of weeks, these symptoms return if not treated with antibiotics. The 100% rating for this condition continues only while the condition is active. After that, any remaining side effects or symptoms are rated separately. These symptoms could include liver damage, code 7312, spleen damage, codes 7706-7707, or nerve damage. The code for nerve damage depends on which nerve is affected and the severity of the damage. Thorough information on rating nerve damage can be found on The Central Nervous System page.
Code 6309: Rheumatic fever is a disease that affects the tissues of the body, causing them to swell. It can damage the valves of the heart, which can cause congestive heart failure. Symptoms also include rashes, twitching in the face and arms, and fevers. The 100% rating for this condition continues only while the condition is active. After that, any remaining side effects or symptoms are rated separately. These symptoms could include heart damage, code 7020.
Code 6311: Miliary tuberculosis is tuberculosis that began in the lungs but then traveled to other parts of the body. This condition would be rated for both pulmonary and nonpulmonary tuberculosis. (Their 100% ratings, however, cannot be combined during the 1-year period after inactivity. Their symptoms or complications, however, can be rated during that period instead of waiting for reevaluation at the 1-year mark).
Code 6312 did not exist before this date.
Code 6316: Brucellosis is a bacterial infection that causes fevers, headaches, depression, and weakness. The symptoms can come and go throughout the rest of your life if the disease is not properly treated with antibiotics. The 100% rating for this condition continues only while the condition is active. After that, any remaining side effects or symptoms are rated separately. These symptoms could include liver damage, code 7312, or meningitis, code 8019.
Code 6317: Scrub typhus is an infection caused by parasites that can be treated with antibiotics, although many strains are not responsive to treatments. The 100% rating for this condition continues while the condition is active and for the first 3 months following. After that, any remaining side effects or symptoms are rated separately. These symptoms could include skin damage, codes 7800–7805, and spleen damage, codes 7706-7707.
Code 6318: Melioidosis is a bacterial infection that causes pain, coughing, pneumonia and skin infections. The 100% rating for this condition continues only while the condition is active. After that, any remaining side effects or symptoms are rated separately. These symptoms could include arthritis, code 5003, lung tissue damage, code 6825, or meningitis, code 8019.
Code 6319: Lyme disease is a bacterial disease common in the US and spread by ticks. Symptoms include fever, skin rash, fatigue, and depression and can affect the joints, heart and nerves if it is not treated properly. The 100% rating for this condition continues only while the condition is active. After that, any remaining side effects or symptoms are rated separately. These symptoms could include arthritis, codes 5002–5003, heart damage, code 7020, chronic fatigue, code 6354, and nerve damage.
Codes 6325, 6326, 6329, 6330, 6331, 6333, 6334, and 6335 did not exist before this date.
Code 6351: HIV (human immunodeficiency virus) is a virus mostly spread by sexual contact with an infected person, although it can also be spread from mother to child or by contact with infected blood. The virus attacks “T4” cells that support the immune system of the body, thus causing the body to be very vulnerable to infections, other diseases (“secondary diseases”), and cancers. The HIV virus can cause the disease AIDS (acquired immunodeficiency syndrome). It takes many years for an HIV infection to develop into AIDS. The presence of AIDS is confirmed if the T4 cell count is less than 200.
If a higher rating can be received by rating a secondary disease or infection than can be received by rating HIV or AIDS, then it can be rated under that secondary condition. A rating for both, however, is not allowed—only a rating for HIV or a rating for ONE of the secondary conditions, whichever can provide the higher rating. If it is rated on one of the secondary conditions, then the final code will look like this: 6351-4901. The first four-digit code defines the condition as HIV, and the second four-digit code tells how the condition is rated.
The ratings:
If there is an active AIDS disease with either regularly occurring infections/diseases or infections/diseases in numerous areas of the body, it is rated 100%. A 100% rating is also given for HIV if there is a secondary disease that is present the majority of the time and causes continual weight loss.
If there is a secondary disease, infection, or Neoplasm as a result of AIDS, then the minimum rating is 60%. This rating is also given if there are significant symptoms throughout the body that cannot be controlled, diarrhea, and weight loss.
If the HIV is being treated by “approved” medication (medications that are prescribed for research by a qualified medical institution), but there are still regularly occurring symptoms throughout the body and intermittent diarrhea, then it is rated 30%. This rating is also the minimum rating given if the T4 cell count is less than 200, there is Hairy Cell Leukoplakis, or Oral Candidiasis.
If the HIV is being treated by “approved” medication, there are at least definite symptoms present, and the T4 cell count is between 200 and 500, then it is rated 10%. If there are clear signs of depression or memory loss that interfere with the ability to work, a rating of 10% may also be given.
If there are no symptoms that affect the ability of the individual to function, then it is rated 0%, even if there is a decreased T4 cell count, disease in the lymph nodes, or diagnosed AIDS.
December 9, 2018 – The Hemic and Lymphatic Systems
Code 7700: Anemia that is caused by low levels of iron or B12 in the body is rated under this code. This condition is rated based on the amount of Hemoglobin in the blood and symptoms directly related to it. If the anemia causes other complications, like dementia or neuropathy, that are not rated under this code, then those conditions can be rated separately.
The normal hemoglobin level for an adult female is 12 to 16 grams per 100 milliliters of blood (g/dL). For an adult male it is 13.5 – 17.5 g/dL. If the hemoglobin level in the blood is 5 g/dL or less and causes symptoms like difficulty breathing or Congestive Heart Failure, then it is rated 100%. If the hemoglobin level is 7 g/dL or less and causes symptoms like difficulty breathing, an enlarged heart, high blood pressure, or fainting (at least 3 times in the last 6 months), then it is rated 70%. If the hemoglobin level is 8 g/dL or less and causes symptoms like weakness, headaches, fatigue, lightheadedness, or shortness of breath, then it is rated 30%. If the hemoglobin level is 10 g/dL or less and causes symptoms like weakness, fatigue or headaches, then it is rated 10%. If the hemoglobin level is 10 g/dL or less but does not cause any symptoms, then it is rated 0%.
It is important to note that these ratings are based on the hemoglobin level and the symptoms. After the hemoglobin level for each rating, it says “or less,” meaning that if the condition has an enlarged heart (rated 70%) and the hemoglobin level is 5gm/100ml (rated 100%), then the rating would only be 70% since the hemoglobin level for 70% states 7gm/100ml or less. Regardless of how low the hemoglobin level is, the rating can only go up if the symptoms support it. On the contrary, if the hemoglobin level is higher than the requirement for a particular rating, then it cannot receive a lower rating. For example, if the hemoglobin level is 8gm/100ml (rated 30%) and there is an enlarged heart (rated 70%), the rating would only be 30% since the hemoglobin level is too high for the 70% rating. Finally, if there is a significant heart condition, but only mild anemia, then the condition is only rated on the heart condition under a heart code.
Code 7702: Agranulocytosis (also known as granulopenia and agranulosis) is a condition where the bone marrow does not produce enough white blood cells. This significantly decreases the body’s immune system and makes the body very vulnerable to infection and disease. If the condition requires a bone marrow transplant, it is rated 100%. This 100% rating continues for 6 months following the transplant. The condition will then be reevaluated and re-rated.
Whether or not a transplant is performed, if the condition requires a transfusion of platelets or red blood cells at least once every 6 weeks, or if infections occur at least once every 6 weeks, it is rated 100%. If a transfusion or an infection occurs at least once every 3 months, then it is rated 60%. If a transfusion or an infection occurs at least once a year, then it is rated 30%. If the condition at least requires continuous medication, then it is rated 10%.
Code 7703: Leukemia is a cancer of the blood or bone marrow that causes the over-production of immature white blood cells. There are many different kinds of leukemia, but all are rated the same. If it is active and undergoing treatment, then it is rated 100%. This 100% rating continues for 6 months after the last treatment. Then the condition will be reevaluated and re-rated. If the leukemia is not active or being treated, then it is rated as anemia or aplastic anemia, whichever gives the higher rating. The final code would look like this: 7703-7700. The first four-digit code defines the condition as leukemia, and the second four-digit code says that it is rated as anemia.
Code 7704: Polycythemia vera is the opposite of anemia. Instead of having too few red blood cells, the bone marrow produces too many red blood cells. This can cause shortness of breath, bleeding, dizziness and many serious symptoms. If this condition causes a serious side effect like high blood pressure, gout, a stroke or a blood clot, then those conditions are rated separately. They must be serious enough to cause a significant decrease in the ability to function in order to qualify for a rating. For example, slightly high blood pressure that does not limit the amount of activity a person can do is not enough for high blood pressure to be rated separately.
Polycythemia vera is not curable but can be treated. If it requires treatment of Myelosuppressants then it is rated 100%. This 100% rating continues for 3 months following the last myelosuppressant treatment. The condition is then reevaluated and re-rated.
Whether or not myelosuppressants were used, if the condition is severe enough that a Phlebotomy has to be routinely performed, then it is rated 40%. If the condition is stable whether or not medication is being taken, then it is rated 10%.
Code 7705: Thrombocytopenia is a condition where the platelet count in the blood is low. The normal amount of platelets in a microliter of blood is between 150,000 to 450,000. If the platelet count is less than 20,000 and there is bleeding that requires medication and transfusions, then it is rated 100%. If the count is between 20,000 and 70,000 but there is no bleeding and it does not require treatment, then it is rated 70%. If the platelet count is stable and between 70,000 and 100,000 and there is no bleeding, then it is rated 30%. A stable count of 100,000 or more with no bleeding is rated 0%.
Code 7712 did not exist before this date.
Code 7714: Sickle cell anemia is a kind of anemia where the red blood cells that carry the oxygen become shaped like a sickle (or a boomerang). Because of this, they are not able to carry as much oxygen to the body, and they sometimes get stuck in small blood vessels, blocking the blood flow to the tissues. A diagnosis of this condition alone is not enough to get a rating. There must be proof of significant symptoms that limit your ability to function in some way. This condition is genetic, and so it technically did exist prior to service (EPTS), and may not be ratable by the DoD.
If there are regular severe painful episodes, blood clots, and other symptoms that all cause the condition to be severe enough that even light manual labor cannot be performed, then it is rated 100%. If there are severe painful episodes multiple times a year with symptoms that restrict activity to just light manual labor, then it is rated 60%. If there have been episodes of severe active destruction of red blood cells and these episodes cause symptoms that continue after the episode is over, then it is rated 30%. If the condition has been properly diagnosed and it affects some organs, but there are no symptoms, then it is rated 10%.
Code 7715: Lymphomas that are not Hodgkin’s are rated under this code. Lymphomas are the growth of lymphoid cells in areas they are not meant to be. If the cancer is active or undergoing treatment, then it is rated 100%. This rating continues for 6 months following the last treatment. It is then reevaluated and re-rated based on the ongoing symptoms.
Code 7716: Aplastic anemia is a condition where the bone marrow does not make enough new blood cells. If the condition requires a bone marrow transplant, then it is rated 100%. This 100% rating will continue for 6 months following the transplant surgery. After this time, the condition will be reevaluated and rated on its need for continuing transfusions or medications as detailed below.
If the condition does not need a transplant, but requires a transfusion of red blood cells or platelets at least once every 6 weeks or if there are infections that occur at least every 6 weeks, then it is rated 100%. If it requires a transfusion at least once every 3 months or if there are infections occurring every 3 months, then it is rated 60%. If it requires a transfusion at least once a year or if there are infections occurring at least once a year, then it is rated 30%. If the condition at least requires continuous medication, then it is rated 10%.
Code 7718 did not exist before this date.
Code 7719 did not exist before this date.
Codes 7720-7723 did not exist before this date.
Code 7724 did not exist before this date.
Code 7725 did not exist before this date.
August 13, 2018 – The Skin
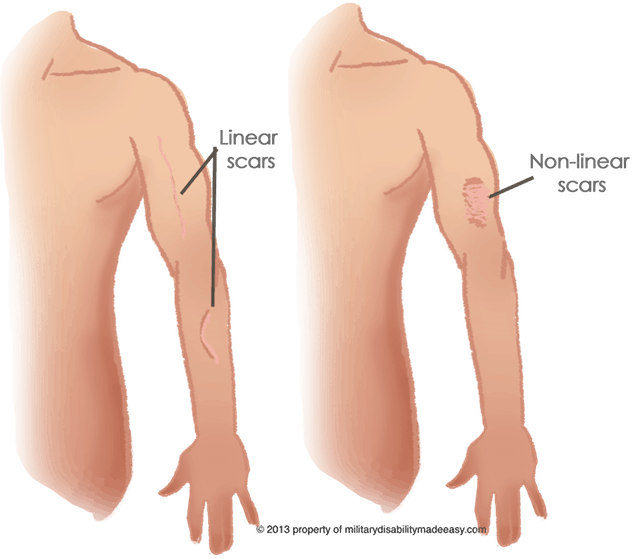
Non-Linear Scars of the Body
Non-linear scars are scars that are patches, not thin lines.
Important! Each part of the body that is affected by a non-linear scar IS rated separately! Woo-hoo! When the ratings are assigned, numerous ratings under these codes can be given. So, if more than one rating is given under code 7801, then it should be clear on the rating decision which area each rating is for.
Below is a picture of the different areas of the body that can be rated separately. There are 6 areas in total, and they include the right arm, the left arm, the right leg, the left leg, the front of the torso, and the back of the torso. The front and back of the torso are separated by the midline on the side of the body. (The neck and head are rated under code 7800).
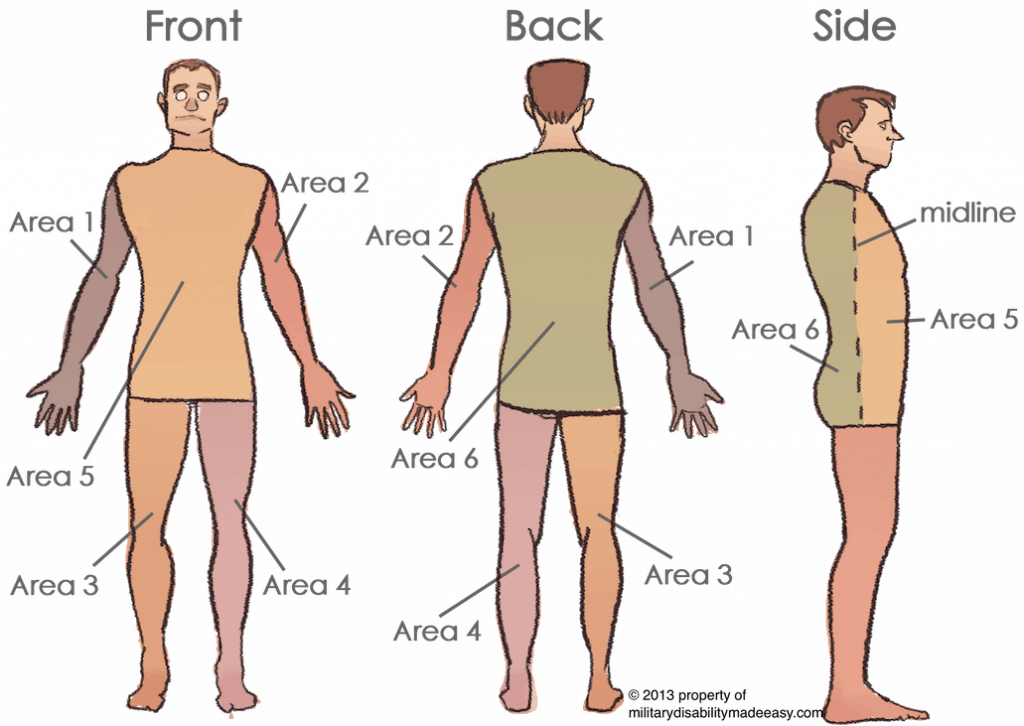
It is important that each of these areas is clearly defined and measured so that the overall rating is accurate.
All non-linear scars of the body are rated based on the area (square inches, in2) of the skin affected. These calculations can be a bit complicated to measure, and may vary based on the examining physician (unfortunately). You can help yourself, however, by knowing exactly how these measurements should be done.
To measure the area of skin affected by a burn, measure the length (top-to-bottom) and width (side-to-side) and then multiply them together. It may be necessary to portion the scar into sections that are then measured and their areas added together. For example, see the scar in the picture below.
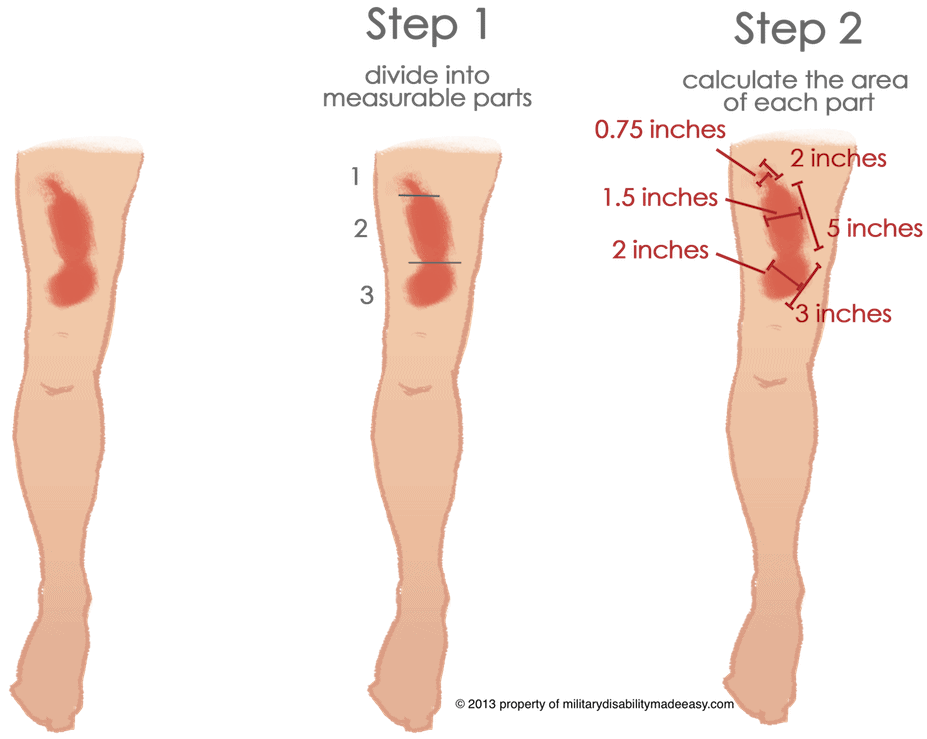
Since this scar curves, it is impossible to measure the exact area it affects if measured all at once. It can, however, be pretty easily divided into three parts. Part 1 is 2 inches long and ¾ inch wide at its widest part. This makes the area 1.5 in2 (¾ x 2 = 1.5 in2). Part 2’s area is 7.5 in2 (1.5 x 5 = 7.5 in2). Likewise, part 3’s area is 6 in2 (3 x 2 = 6 in2). To then get the total area of scarring on that leg, add the three areas together: 1.5 + 7.5 + 6 = 15 in2.
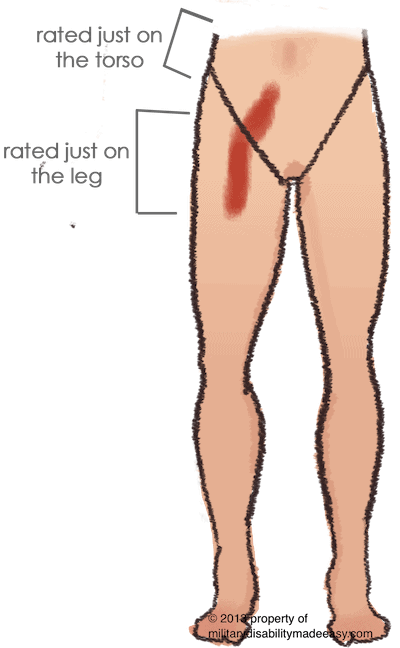
If a single scar runs across one part of the body and into another, then it is divided and rated for each bit of it that is in each part of the body. Unfortunately, this could decrease the overall rating if the parts of the scar in each area are smaller, and thus rated less, than it might have been as a whole. Sorry. In the image to the right, the scar would be divided and rated once for the torso and once for the right leg.
Time for ratings:
Code 7801: Deep, non-linear scars are considered “deep” if there is damage to the soft tissues under the skin. If the area of scarring in a single body part is 144 in2 or bigger, then it is rated 40%. If the area is between 72 in2 and 144 in2, it is rated 30%. If the area is between 12 in2 and 72 in2, then it is rated 20%. If it is between 6 in2 and 12 in2, it is rated 10%.
Code 7802: Superficial, non-linear scars are ones that only affect the skin, not the soft tissues underneath. If the area of scarring in a single body part is 144 in2 or more, it is rated 10%. No other rating is given for superficial scars under this code.
Note: If the scars cause other disabling conditions beyond disfigurement (like pain, nerve damage, the inability to properly use an arm, etc.), then those conditions are rated separately. Search for the condition on this site, and then rate accordingly.
Linear Scars of the Body
Code 7805: Linear scars are lines (not necessarily straight) instead of patches. These scars are not ratable in and of themselves. If they cause another condition that makes it hard to properly do your job, then that other condition is rated. So, for example, if a linear scar running up the arm makes it impossible to fully bend or straighten the arm at the elbow, then it is rated under limited motion of the elbow. The final code will look like this: 7805-3400. The first four-digit code defines the condition as a linear scar, and the second four-digit code tells how it is rated.
Skin Conditions
Code 7806: Dermatitis and eczema are essentially the same thing, although some doctors might describe them slightly different. For rating purposes, however, they are treated the same. Basically, dermatitis is a condition where the skin swells and turns red—the standard rash.
There are three different rating options for this condition. If the condition is so severe that it causes permanent scars, it can be rated as a scar condition. The final code in that case would look like this: 7806-7801. The first four-digit code defines the condition as dermatitis, and the second four-digit code tells how it is rated.
It can also be rated under this code either on calculations/estimations or on the required treatment of the condition itself.
Calculations/estimations: If there is more than 40% of total body or more than 40% of exposed divisions affected, it is rated 60%. If there is 20% to 40% of total body or 20% to 40% of exposed divisions affected, it is rated 30%. If there is 5% to 20% of total body or 5% to 20% of exposed divisions affected, it is rated 10%. If there is less than 5% of total body or less than 5% of exposed divisions affected, it is rated 0%.
Treatments: If the condition required the almost constant use of oral or injected medications to regulate the immune system over the past 12 months (methotrexate, steroids, etc.), it is rated 60%. If the condition required oral or injected medications to regulate the immune system for a total of 6 weeks or more during the past 12 months, it is rated 30%. If the condition required oral or injected medications to regulate the immune system for a total of less than 6 weeks over the past 12 months, it is rated 10%. If the condition only required Topical medications over the past 12 months, it is rated 0%.
Code 7809: Lupus is a condition where the immune system attacks the healthy cells of the skin, causing severe sores, tearing, and scarring of the skin. Most often, these occur on the head near the ears, eyes, nose, lips and cheeks, but in some cases lupus sores can affect other areas of the body. Lupus is either rated as dermatitis or as scars/disfigurement, whichever best describes the disability. The final code will look like this: 7809-7801. The first four-digit code defines the condition as lupus, and the second four-digit code tells how it is rated.
If the lupus affects parts of the body besides the skin, then it is rated under code 6350 for systematic lupus erythematosus. A rating cannot be given under both codes. Only one or the other.
If the lupus is caused by tuberculosis, it is rated under the next code.
Code 7813: Dermatophytosis (“ringworm”) is a fungal infection that causes ring-shaped red and swollen patches on the skin. This condition is either rated under dermatitis or scars/disfigurement whichever best describes the disability. The final code will look like this: 7813-7801. The first four-digit code defines the condition as dermatophytosis, and the second four-digit code tells how it is rated.
Codes 7815, 7816, and 7821 are all rated on the same rating system.
Code 7815: Bullous disorders cause blisters of clear liquid to form in between the layers of the skin, most often on the inner thighs and upper arms.
Code 7816: Psoriasis is an autoimmune condition that tells the body to produce more skin cells even though they are not needed. This can cause numerous different things to happen to the skin, including redness, swelling, scaly texture, patches of red bumps, and more.
Code 7821: Cutaneous manifestations of collagen-vascular diseases are skin conditions that occur when the immune system attacks the collagen. Collagen is all the proteins that are in the skin. Psoriasis is considered a collagen-vascular disease. This code is used to rate any collagen-vascular disease that is not rated elsewhere.
The ratings:
There are three different rating options for these conditions. If the condition is so severe that it causes permanent scars, it can be rated as a scar condition. The final code in that case would look like this: 7816-7801. The first four-digit code defines the condition as one of the above conditions, and the second four-digit code tells how it is rated.
These conditions can also be rated under their own codes either on calculations/estimations or on the required treatment of the condition itself.
Calculations/estimations: If there is more than 40% of total body or more than 40% of exposed divisions affected, it is rated 60%. If there is 20% to 40% of total body or 20% to 40% of exposed divisions affected, it is rated 30%. If there is 5% to 20% of total body or 5% to 20% of exposed divisions affected, it is rated 10%. If there is less than 5% of total body or less than 5% of exposed divisions affected, it is rated 0%.
Treatments: If the condition required the almost constant use of medications to regulate the immune system (methotrexate, steroids, etc.) over the past 12 months, it is rated 60%. If the condition required medications to regulate the immune system for a total of 6 weeks or more during the past 12 months, it is rated 30%. If the condition required medications to regulate the immune system for a total of less than 6 weeks over the past 12 months, it is rated 10%. If the condition only required Topical medications over the past 12 months, it is rated 0%.
Code 7817: Exfoliative dermatitis (erythroderma) is a dermatitis that causes a scaly rash that covers the majority of the entire body. It is normally caused by another condition, like cancer or a reaction to a medication. If that condition is unfitting by itself, then the exfoliative dermatitis can only be rated as well if it contributes significantly to making the service member Unfitting (super sensitive to motion, can’t wear their uniform, etc.).
If the majority of the skin is affected and things such as weight loss, fever, low protein in the blood, etc., are present, and continuous medications to regulate the immune system (methotrexate, steroids, etc.) were taken over the past 12 months or regular treatments of ultraviolet or other light wave/beam therapy were needed during the past 12 months, it is rated 100%.
If the majority of the skin is affected, and continuous medications to regulate the immune system were taken over the past 12 months or regular treatments of ultraviolet or other light wave/beam therapy were needed during the past 12 months, it is rated 60%.
Regardless of how much skin is affected, if medication to regulate the immune system or ultraviolet or other light wave/beam therapy was needed for a total of 6 weeks (does not need to be consecutive) or more during the past 12 months, it is rated 30%.
Regardless of how much skin is affected, if medication to regulate the immune system or ultraviolet or other light wave/beam therapy was needed for a total of less than 6 weeks (does not need to be consecutive) or more during the past 12 months, it is rated 10%.
Regardless of how much skin is affected, if only Topical treatments were used during the past 12 months, it is rated 0%.
Code 7820: All other infections of the skin that are not listed elsewhere are rated under this code. These conditions are either rated as dermatitis or as scars/disfigurement, whichever best describes the disability. The final code will look like this: 7820-7801. The first four-digit code defines the condition as a skin infection, and the second four-digit code tells how it is rated.
Code 7821: Cutaneous manifestations of collagen-vascular diseases are skin conditions that occur when the immune system attacks the collagen. Collagen is all the proteins that are in the skin. Psoriasis is considered a collagen-vascular disease. This code is used to rate any collagen-vascular disease that is not listed elsewhere.
Code 7822: Any other skin conditions that cause hard, scaly bumps (“papulosquamous disorders”) to form on the skin that are not listed anywhere else on this page are rated under this code.
There are three different rating options for these conditions. If the condition is so severe that it causes permanent scars, it can be rated as a scar condition. The final code in that case would look like this: 7822-7801. The first four-digit code defines the condition as one of the papulosquamous disorder, and the second four-digit code tells how it is rated.
These conditions can also be rated under this code either on calculations/estimations or on the required treatment of the condition itself.
Calculations/estimations: If there is more than 40% of total body or more than 40% of exposed divisions affected, it is rated 60%. If there is 20% to 40% of total body or 20% to 40% of exposed divisions affected, it is rated 30%. If there is 5% to 20% of total body or 5% to 20% of exposed divisions affected, it is rated 10%. If there is less than 5% of total body or less than 5% of exposed divisions affected, it is rated 0%.
Treatments: If the condition required the almost constant use of medications or light therapy over the past 12 months, it is rated 60%. If the condition required medications or light therapy for a total of 6 weeks or more during the past 12 months, it is rated 30%. If the condition required medications or light therapy for a total of less than 6 weeks over the past 12 months, it is rated 10%. If the condition only required Topical medications over the past 12 months, it is rated 0%.
Code 7824: Diseases of keratinization affect the process where the lower layers of the skin turn into the harder outer layer of skin. Keratin is the protein that causes the skin to harden. Any condition that affects the process of keratinization is rated under this code.
If the condition affects the whole body and required almost constant oral or injected medication over the past 12 months, it is rated 60%. If the condition affects the whole body and required the use of oral or injected medication for a total of at least 6 weeks during the past 12 months, it is rated 30%. If the condition only affects some areas of the body and required the use of oral or injected medication for a total of less than 6 weeks during the past 12 months, it is rated 10%. If only Topical treatments were required during the past 12 months, it is rated 0%.
Code 7825: Chronic hives are pale red, itchy bumps on the skin that are caused either by allergic reactions or various other causes. To qualify as chronic, they must last for 6 weeks or more. If there were severe debilitating episodes that occurred at least 4 times over the past 12 months that could not be controlled by treatment, it is rated 60%. If there were severe Debilitating episodes that occurred at least 4 times over the past 12 months but it could be controlled by medications that regulate the immune system (methotrexate, steroids, etc.) it is rated 30%. If there were episodes (not debilitating) that occurred at least 4 times over the past 12 months, but the condition could be controlled by medications that control swelling, it is rated 10%.
Code 7826: Primary cutaneous vasculitis is a condition of the small blood vessels near the skin, which causes them to burst. The skin turns red or purple due to bleeding under the skin. If this condition is caused by other conditions, like infections, medications, cancer, autoimmune disorders, etc., it can only be rated as that condition. If it is not caused by another condition, then it can be rated here. Likewise, if the condition caused significant scarring, it can be rated under one of the scar codes. Choose the one rating system that would give the highest rating.
If there were at least 4 Debilitating episodes over the past 12 months that did not respond to treatment, it is rated 60%. If there were at least 4 debilitating episodes over the past 12 months that were controlled by medications that regulate the immune system (methotrexate, steroids, etc.), then it is rated 30%. If there were 1 to 3 episodes (not debilitating) over the past 12 months that were controlled by medications that regulate the immune system, then it is rated 10%.
Code 7827: Erythema multiforme (toxic epidermal necrolysis, “TENs”) is either caused by an infection or is a reaction to medication. It causes red skin rashes and bumps to appear all over the body. It then attacks and kills the skin all over the body, causing the top layer of skin to detach from the lower layers, which can send the organs into failure. If the condition caused significant scarring, it can either be rated as a scar or under this code. Choose the one that would give the highest rating.
If there were severe Debilitating episodes that occurred at least 4 times over the past 12 months that could not be controlled by treatment, it is rated 60%. If there were episodes (not debilitating) that occurred at least 4 times over the past 12 months but it could be controlled by medications that regulate the immune system, it is rated 30%. If there were episodes (not debilitating) that occurred 2 or 3 times over the past 12 months that were controlled by medications that control swelling, it is rated 10%. A 10% rating is also given if there were 1 to 3 episodes that occurred over the past 12 months that were controlled by medications that regulate the immune system.
Codes 7828 and 7829 are rated on the same system below.
Code 7828: Acne is a skin condition that causes pus-filled raised bumps that can occur anywhere on the body.
Code 7829: Chloracne is a condition where acne erupts over patches of skin that have come in contact with chemicals that contain dioxins.
Some acne is very superficial, involving only one layer of the skin, while other acne can be very deep. Often acne causes scarring. If the scars are the main disability, then this condition can be rated under a scar code.
The ratings: If the acne is deep, causing inflammation and pus-filled cysts, and affects 40% or more of the face and neck, it is rated 30%. If the acne is deep, causing inflammation and pus-filled cysts, and affects less than 40% of the face and neck, or if deep acne is in areas other than the face and neck, it is rated 10%. If the acne is superficial, it is rated 0%.
May 13, 2018 – The Eyes
Visual Field Rating System
The visual field is the entire range of vision that can be seen when looking at a fixed point straight ahead. Visual field testing is performed using several different Automatic Tests. These tests chart the range of vision of each eye without moving the eyeball. A copy of these results is also essential to rating. The chart must be in the medical records.
Muscle Dysfunction Rating System
The examining optometrist must chart any decrease in muscle function in all four quadrants on a Goldmann perimeter chart in order for the condition to be rated.
Eye Conditions
Codes 6000-6009 are either rated on the Visual Impairment Rating System or on incapacitating episodes, whichever gives the higher rating. Incapacitating episodes:
An “incapacitating episode” is a period of severe symptoms that requires bed rest and treatment prescribed by a physician. If the physician did not prescribe bed rest, it is not considered an incapacitating episode.
If there were incapacitating episodes adding up to 6 weeks or more during the last 12 months, it is rated 60%. If the incapacitating episodes over the last 12 months add up to 4 to 6 weeks, it is rated 40%. Two to 4 weeks is rated 20%, and 1 to 2 weeks is rated 10%.
Code 6009: All other unhealed eye injuries are rated under this code.
Code 6011: Any retina condition (scars, atrophy, etc.) not rated in the Diseases of the Eye section is rated under this code. If the condition causes irregular vision with double images, extra large images, extra small images or other irregularities, it is rated 10%. This 10% rating is given whether there is one eye or both eyes affected. The condition can be rated on the Visual Impairment Rating System if it would receive a higher rating.
Code 6012: Angle-closure glaucoma (or closed-angle glaucoma) is a condition where the optic nerve is damaged, normally by high fluid pressure in the eye, causing loss of vision. It is very sudden and painful, and the loss of vision can occur very quickly if not treated right away. This condition is either rated on the Visual Impairment Rating System or on incapacitating episodes (below), whichever results in the higher rating.
An incapacitating episode is defined as a period of severe symptoms that requires bed rest prescribed by a physician. If the physician did not prescribe it, then it does not qualify to be rated as an incapacitating episode. If there were incapacitating episodes that equal a total of 6 weeks or more during the past 12 months, it is rated 60%. If the episodes equal a total of 4-6 weeks during the past 12 months, it is rated 40%. If they equal a total of 2-4 weeks during the past 12 months, it is rated 20%. The minimum rating is 10% if medication is constantly needed to control the symptoms.
Code 6013: Open-angle glaucoma is a condition where the optic nerve is damaged, normally by high fluid pressure in the eye, causing loss of vision. Unlike angle-closure glaucoma, it progresses slowly over time and is harder to detect before significant vision loss occurs. This condition is rated on the Visual Impairment Rating System. If continuous medication is required for the condition, the minimum rating is 10%.
Code 6014: Malignant tumors of the eyeball itself are rated under this code. If other things are also affected by the cancer, then each system can be rated separately. So, if the cancer is in the eye and the surrounding skin, then the eye and the skin are each rated separately.
If the cancer is active, and requires chemotherapy, x-ray therapy, surgery, or similar treatments to more than just the eye area, it is rated 100%. This 100% rating will continue for the first 6 months following the completion of the any treatment. The condition will then be reevaluated and rated based on any continuing symptoms, like vision loss.
If the cancer is active, but does not require chemotherapy, x-ray therapy, surgery, or similar treatments to more than just the eye area, then each symptom, like visual impairment, muscle impairment, or disfigurement, is individually rated.
Code 6015: All other benign tumors affecting the eye are rated under this code and can be rated two times. Once for any effect it has on visual ability, and once for any nonvisual impairment like disfigurement.
Code 6017: Trachomatous conjunctivitis is the swelling of the conjunctiva due to a bacterial infection, that continues despite treatment. This is not pink eye. Pink eye is caused by a viral infection and is rated below.
If the condition is currently active, it is rated on any visual impairment. The minimum rating for this condition is 30%. So regardless of the severity of visual impairment, it will at least be rated 30%. If the condition is not currently active, then it is rated on any lasting symptoms.
Code 6018: All other conjunctivitis conditions are rated under this code. Conjunctivitis can be caused by many things including reactions to chemical exposure and viruses. Viral conjunctivitis is popularly known as “pink eye.” Conjunctivitis is not ratable unless it is chronic—lasts a long time and is not responsive to treatment, or regularly returns despite treatment.
If the conjunctivitis is currently active with symptoms like redness, irritation, seeping, etc., it is rated 10%. If it is not active, it is rated on any lasting symptoms like visual impairment.
Code 6026: Optic neuropathy is basically damage to the optic nerve. Any optic nerve damage that is not caused by high fluid pressure (glaucoma) is rated under this code. This condition is rated on the Visual Impairment Rating System.
Code 6027: A cataract occurs when the crystalline lens becomes cloudy. It can be slightly cloudy or completely block any light from passing through the lens. This condition can be corrected by surgery. If the surgery has not yet been performed, it is rated on the Visual Impairment Rating System.
If the surgery has been performed, it is still rated on the Visual Impairment Rating System, however it is important to note that the visual field will be measured differently depending on the outcome of the surgery. If a replacement lens is in place (“pseudophakia”) and functions normally, then the ring (isopter) used to rate the condition is the III4e. If it is in place but does not function normally, the ring used to rate it is IV4e. See the lens discussion under the Visual Field Rating System for more specific information.
If a replacement lens was not implanted, then the condition is rated as aphakia.
Code 6034: Pterygium is a condition where benign fibers of the conjunctiva grow into the cornea. This condition is either rated on visual impairment, disfigurement, or conjunctivitis, whichever most closely reflects the symptoms of the condition.
Code 6035: Keratoconus is a condition where the cornea gradually changes its shape, causing significant vision problems. This condition is rated on the Visual Acuity Rating System. Since the VASRD clearly states that this condition is to be rated on visual acuity, it cannot also be rated for visual field or muscle dysfunction unless they are caused by an entirely different condition.
Code 6036: A corneal transplant is rated on the Visual Impairment Rating System. If there is also pain and sensitivity to light, the minimum rating for this condition is 10%.
Code 6091: Symblepharon occurs when the lining of the eyelid attaches to the conjunctiva because of injury or disease. This restricts the movement of the eye and the ability to open the eyelid. It is either rated on visual impairment, the inability to close the eyelids (code 6022), disfigurement (code 7800), or on other symptoms. Each symptom can be rated separately.
May 13, 2018 – The Female Reproductive System and Breasts
Code 7619: The removal of one or both ovaries is rated 100% for the first 3 months after surgery. After that period, the complete removal of both ovaries is rated 30%. Anything less than the complete removal of both ovaries is rated 0%.
Code 7621: If the uterus slips down completely through the vagina, then it is rated 50%. If it slips down only partially through the vagina, then it is rated 30%.
Code 7622: If the uterus does not slip down, but is significantly out of place, then it is rated under this code. If the displacement causes constant or frequent problems with menstrual periods, then it is rated 30%. If the displacement causes Adhesions, and the menstrual periods are irregular, then it is rated 10%.
Code 7623: If pregnancy causes the wall between the vagina and the rectum to tear, resulting in a Rectocele, or if it causes the wall between the bladder and the vagina to tear, resulting in a Cystocele, it is rated 50%. If the pregnancy causes the vagina to be loose or gaping, then it is rated 10%.
Note: Codes 7622 and 7623 were combined with 7621 and now all conditions previously covered by these codes are all rated under 7621.
Code 7628: Tumors affecting the breast or the reproductive organs are rated based on how they affect the systems around them. For example, if the condition interferes with the ability to urinate, then it would be rated under that symptom. The final code for this condition will be a hyphenated Analogous code that would look like this: 7628-3009. The first four-digit code tells us that the condition is benign cancer of the reproductive system, and the second four-digit code is the code the condition is actually rated under.
Code 7627: Cancer affecting the breast or the reproductive organs that is active is rated 100%. This 100% rating will continue for the first 6 months after the last treatment. The condition will then be reevaluated. If it is no longer active, then it will be rated on any lasting symptoms just like any benign condition.
December 10, 2017 – Endocrine System Conditions and Hyperthyroid Heart Disease
Code 7900: Hyperthyroidism occurs when the thyroid produces too many hormones. This causes all the functions in the body to speed up, which can cause symptoms like tremors, hair loss, nervousness and anxiety, rapid heart rate, eye swelling, vomiting, and muscle weakness. Most severely symptomatic patients would be treated to stop the excessive production of thyroid hormones, therefore any permanent rating over 10% is very unusual.
If the only significant symptom of this condition is heart disease, then it can be rated under code 7008 if that would produce a higher rating than one under this code. Likewise, if the only significant symptom is problems with the eyes, then rate it under the eye condition closest to the symptom.
If the thyroid is swollen, the heart rate is faster than 100 beats per minute, there are eye problems, weakness, weight loss and other symptoms of the cardiovascular system, nervous system, or gastrointestinal system then it is rated 100%.
If you have unstable emotions, a fast heart rate, you get tired and weak easily, and have an increased pulse or blood pressure, it is rated 60%. If you have a fast heart rate, tremors (most often in the hands), and an increased pulse or blood pressure, it is rated 30%. If you have an occasionally fast heart rate and tremors, or if constant medication is required to control the condition then it is rated 10%.
Code 7901: A toxic adenoma of the thyroid gland is a tumor in the thyroid that causes it to produce too many hormones. This causes all the functions in the body to speed up, which can cause symptoms like tremors, hair loss, nervousness and anxiety, rapid heart rate, eye swelling, vomiting, and muscle weakness. Most severely symptomatic patients would be treated to stop the excessive production of thyroid hormone, therefore any permanent rating over 10% is very unusual.
If the only significant symptom of this condition is heart disease, then it can be rated under code 7008 if that would produce a higher rating than one under this code. Likewise, if the only significant symptom is problems with the eyes, then rate under the eye condition closest to the symptom.
The ratings: If the thyroid is swollen, the heart rate is faster than 100 beats per minute, there are eye problems, weakness, weight loss and other symptoms of the cardiovascular system, nervous system, or gastrointestinal system, then it is rated 100%.
If you have unstable emotions, a fast heart rate, you get tired and weak easily, and have an increased pulse or blood pressure, it is rated 60%. If you have a fast heart rate, tremors (most often in the hands), and an increased pulse or blood pressure, it is rated 30%. If you have an occasionally fast heart rate and tremors, or if constant medication is required to control the condition then it is rated 10%.
Code 7902: A nontoxic adenoma of the thyroid gland is a tumor that does not cause the thyroid to over-produce hormones. If there is disfigurement of the head or neck, it is rated 20%. Without disfigurement, it is rated 0%. If the tumor causes problems from pushing on the organs or bodily systems around it, then it can be rated based on the problems it causes if their ratings would give a higher rating than 20%. This condition can only be rated once, however. A rating under this code and a rating under a code for a symptom the tumor causes is not allowed.
Code 7903: Hypothyroidism is the opposite of hyperthyroidism in that the thyroid does not produce enough thyroid hormone. This can cause symptoms like constipation, weight gain, tiredness, depression, and muscle cramps. Once again, this condition is very easy to treat with medications (Synthroid, Cytomel, levothyroxine), which generally satisfactorily control all the symptoms. A permanent rating over 10% is again unusual.
If you cannot stand the cold, have muscle weakness, mental issues (depression, dementia, etc.), a slow heart rate (less than 60 beats per minute), drowsiness, and other problems with the heart, it is rated 100%. If there is muscle weakness, mental issues and weight gain, it is rated 60%. If you are easily tired, constipated, and your mind is slow and sluggish, then it is rated 30%. If you are easily tired or if you require constant medication, then it is rated 10%.
Code 7904: Hyperparathyroidism occurs when the parathyroid gland produces too many hormones. There are two kinds of hyperparathyroidism: primary and secondary. Primary is a result of the glands themselves malfunctioning. This kind has very few symptoms but can include symptoms like depression, fatigue, bone pain, and muscle soreness. Secondary is a result of low Vitamin D levels. Symptoms include bone conditions like osteomalacia.
If there are kidney stones, weakness, loss of calcium in the bones, and gastrointestinal symptoms: vomiting, constipation, weight loss, nausea, anorexia, or a peptic ulcer, it is rated 100%. If there are gastrointestinal symptoms and weakness, it’s rated 60%. If constant medication is required to control the condition, it is rated 10%.
If surgery was performed to fix this condition, then the condition can be rated under this code or under any code for a remaining symptom or complication, whichever gives the highest rating. Only one rating can be given.
Code 7905: Hypoparathyroidism occurs when the parathyroid glands produce too few hormones. This causes low levels of calcium in the blood and can cause symptoms like cramping, muscle aches, muscle twitches, headaches, and fatigue. This condition can occur as a side effect from thyroid surgery.
If there are severe muscle twitches, spasms, cramping throughout the body or wheezing in the throat, and either cataracts in the eyes or pressure inside the skull from brain swelling, it is rated 100%. If there is Paresthesia in any of the limbs or around the mouth with cataracts in the eyes or pressure inside the skull, or if there are severe muscle twitches, spasms, cramping or wheezing, it is rated 60%. If constant medication is required to control the condition, it is rated 10%.
Code 7906: Thyroiditis did not exist before this date. This code was created December 10, 2017.
Code 7907: Cushing’s syndrome occurs when there is too much cortisol in the body. Symptoms include rapid weight gain, excessive sweating, easy bruising, weakness, high blood pressure, and more. This condition is most often caused by either a tumor in the pituitary gland (“Cushing’s disease”) or by the prolonged use of steroids to treat other conditions.
If it is an active disease that is getting progressively worse and it causes muscle weakness, osteoporosis, high blood pressure, and the swelling or enlargement of the pituitary or adrenal gland, it is rated 100%. If it is not getting worse and there is muscle weakness and the enlargement of the pituitary or adrenal gland, it is rated 60%. If it causes obesity, a significantly round face caused by weight gain (“moon face”), stretch marks, fragile veins or arteries, and glucose intolerance (a pre-diabetic condition), it is rated 30%.
If the condition is under control or is gone, then left over symptoms or complications are each rated separately.
Code 7908: Acromegaly is a condition where the pituitary gland produces too much growth hormone. This can cause severe disfigurement and Gigantism.
If there is pressure in the skull, which causes problems with things like vision, diseases in the joints, glucose intolerance (hyperglycemia), and either high blood pressure or swelling of the heart, it is rated 100%. If there are diseases in the joints, glucose intolerance, and high blood pressure, it is rated 60%. If there is significant over-growth in the limbs or long bones and an enlarged Sella Turcica, it is rated 30%.
Code 7909: Diabetes insipidus is completely different from diabetes mellitus. It is either caused by the body not producing enough Antidiuretic Hormone or by the kidneys not recognizing and responding properly to that hormone. Without this hormone, much higher levels of water in the body are filtered out through the urine. It causes Polyuria.
If the condition causes polyuria with almost continuous thirst and three or more episodes during the past year of dehydration requiring a replacement of liquids through IV, then it is rated 100%. If the condition causes polyuria with almost continuous thirst and one or two episodes of dehydration requiring a replacement of liquids through IV during the past year, then it is rated 60%. If the condition causes polyuria with almost continuous thirst and one or more episodes of dehydration during the past year that did not require IV treatments, it is rated 40%. If the condition causes polyuria with almost continuous thirst but no episodes of dehydration, it is rated 20%.
Code 7912: Pluriglandular syndrome is any condition that affects multiple glands of the endocrine system at the same time. This condition is rated on the main symptoms it causes. So, if it is tuberculosis that affects numerous glands, then it is rated based on the tuberculosis rating systems. Likewise, if it mainly causes high blood pressure problems, rate it under code 7101. The final code for this condition will look like this: 7912-7101. The first four-digit code defines the condition as pluriglandular, and the second four-digit code tells how it is rated.
Code 7913: Diabetes mellitus is the condition that most of us think of as just diabetes. It occurs either when the pancreas does not produce enough insulin (Type 1), or when the cells do not respond properly to insulin (Type 2). Type 3 diabetes can occur during pregnancy, but this condition resolves after the birth and is not ratable.
Diabetes can affect many different organs including the heart, eyes, and kidneys. It can cause strokes, loss of blood flow to the arms and legs, and nerve dysfunction. It usually takes 10 to 20 years for these secondary conditions to develop.
Note: When rating diabetes mellitus, keep in mind that the secondary conditions of diabetes can be rated separately as long as they are not part of the requirement for a 100% rating. So, if the diabetes is severe enough to warrant a 100% rating under this code, any other conditions that are caused by the diabetes cannot be separately rated. If the diabetes only warrants a 60% rating or lower, however, those other conditions can be rated separately.
Diabetes is rated 100% if all of the following circumstances are present: 1) It requires an insulin injection more than once a day, a restricted diet, and a low physical activity level; 2) It causes three or more hospitalizations each year or requires weekly visits to a care provider; 3) It causes continuous weight loss and weakness.
A 60% rating is given if the condition requires or causes all of the following: 1) insulin; 2) a restricted diet; 3) a low physical activity level; 4) one or two hospitalizations each year or two visits a month to a care provider; 5) minor side effects that would not make a person unemployable without the diabetes.
If the condition requires insulin, a restricted diet, and a low physical activity level, then it is rated 40%.
If the condition requires insulin and a restricted diet, or requires medication taken by mouth and a restricted diet, it is rated 20%.
If it can be managed by a restricted diet alone, it is rated 10%.
Code 7919: C-cell hyperplasia of the thyroid is a condition where the C-cells that produce calcitonin in the thyroid grow abnormally into a cancer. If the cancer is active, it is rated 100%. This 100% rating continues for the first 6 months after the last treatment of procedure. It is then reevaluated. If it is no longer active, then any left over symptoms or complications are rated separately on the function they affect. So if the condition caused high blood pressure, then it would be rated separately.
Code 7008: Hyperthyroid heart disease occurs when the thyroid produces too much thyroid hormone. This can affect the blood pressure, how the heart consumes oxygen, and how much blood the heart can pump. It can be rated only under code 7900 for hyperthyroidism unless Atrial Fibrillation is present. If it is present, then it can either rated under code 7900 or under code 7010 (superventricular arrhythmias), whichever gives the higher rating.
September 10, 2017 – Dental and Oral Conditions
Code 9900: Osteomyelitis or Osteoradionecrosis of the mandible is rated under code 5000, osteomyelitis.
Code 9902: If about half of the mandible is missing and the jaw is unable to move or is limited in its movement, then it is rated 50%. If the jaw motion is not affected, then it is rated 30%.
Code 9903: If the mandible has been broken and did not heal back together, then it is rated 30% for a severe limitation and 10% for a moderate limitation.
Code 9904: If the mandible has been broken and did heal, but not correctly so that there is a definite disfigurement to the bone, then it is rated 20% for severe, 10% for moderate, and 0% for slight.
Code 9905: All other jaw joint conditions (including TMJ) are rated based on limited motion of the joint. The jaw can move in two directions: open and closed, and side-to-side. Only one direction of motion can be rated. If the jaw can’t move side-to-side or open and close, then only the one that will give the higher rating is used.
If the jaw can’t move side-to-side more than 4 millimeters (mm), then it is rated 10%.
If the jaw can’t open more than 10 mm (about 0.4 of an inch), then it is rated 40%. If it can open between 11 and 20 mm (about 0.4 to 0.8 of an inch), it is rated 30%. Between 21 and 30 mm (about 0.8 to 1.2 inches) is rated 20%, and between 31 and 40 mm (about 1.2 to 1.6 inches) is rated 10%.
Code 9906: If more than half of the ramus is missing and the ability to chew or move the jaw is limited, then it is rated 30% for one side and 50% for both sides. If the ability to chew or move the jaw is not limited, then it is rated 20% for one side and 30% for both sides.
Code 9907: If less than half of the ramus is missing but the jaw function is not limited, then it is rated 10% for one side and 20% for both sides.
Code 9911: If half or more of the hard palate is missing and cannot be replaced by a prosthesis, then it is rated 30%. If it can be replaced by a prosthesis, then it is rated 10%.
Code 9912: If less than half of the hard palate is missing and cannot be replaced by a prosthesis, then it is rated 20%. If it can be replaced, it is rated 0%.
Code 9916: If the maxilla has been broken and hasn’t healed back together or has healed incorrectly, then it is rated based on how severely the bone has been disfigured and thus limits its ability to function. If it is severely disfigured, it is rated 30%. If it is moderately disfigured, it is rated 10%. If it is slightly disfigured, it is rated 0%.
August 4, 2014 – Mental Disorders
The VASRD Codes and condition names for Mental Disorders were different before August 4, 2014. The ratings, however, for these conditions did NOT change. Before this date, all Mental Disorders were rated the same as they are now on the current Psychological Rating System.
These are all the Mental Disorders that existed before 2014.
Code 9201: Disorganized schizophrenia is a kind of schizophrenia that causes symptoms of disorganized thought, including bad communication abilities, illogical behaviors and thought processes, a disconnection from emotions, and illogical mumbling. Delusions and hallucinations are often not present in this kind of schizophrenia.
Code 9202: Catatonic schizophrenia is a type of schizophrenia where the mind seems to shut down entirely. People with this condition often do not respond to any type of external stimuli, and will often sit for long periods without moving at all. They can also sometimes have constant twitches, involuntary movements, or repetitive movements. Rarely do they speak, but some can repeat words or phrases.
Code 9203: Paranoid schizophrenia is a type of schizophrenia where the patient believes that they are always in danger and that anyone around them is trying to hurt them. This causes extreme emotional fluctuation, violent behaviors, constant fear, and various delusions.
Code 9204: All other schizophrenic conditions are rated under this code.
Code 9205: This code is used to rate any schizophrenia that has improved. If the person’s condition no longer causes any significant symptoms, then it is rated under this code on whatever symptoms or circumstances still exist.
Code 9208: Delusional disorder is a condition where a person has delusions that are not illogical, just not real. Normally these delusions are small and do not interfere with the person’s overall functioning. A person diagnosed with schizophrenia cannot also be diagnosed with this condition.
Code 9210: All other psychotic disorders are rated under this code.
Code 9211: Schizoaffective disorder is a condition that is a combination of a psychotic disorder and a mood disorder. The mood can be an extreme high or an extreme low or both. In addition to the mood, the individual has flawed mental processes that can cause hallucinations, paranoia, and delusions.
Code 9300: Delirium is a condition characterized by severe confusion. This is often a symptom of Alzheimer’s. It can come on suddenly and last for a few hours or days. Some episodes can be worse than others.
Code 9301: Dementia due to infection is a severe loss of mental ability because of an infection. All areas of mental functioning can be affected by dementia. Symptoms can include memory loss, inability to communicate, confusion, disorientation, loss of logical thinking, etc. For an infection to cause dementia, it must be present over a long period of time. The dementia will slowly develop with the progress of the infection. Infections that can cause dementia include HIV, syphilis, brain infections and more.
Code 9304: Dementia due to head injury is a severe loss of mental ability because of an injury to the brain. All areas of mental functioning can be affected by dementia. Symptoms can include memory loss, inability to communicate, confusion, disorientation, loss of logical thinking, etc. In cases of head injuries, the dementia usually comes on suddenly, but it can also get worse or better over time.
Code 9305: Vascular dementia is a severe loss of mental ability caused by the brain not getting enough blood. All areas of mental functioning can be affected by dementia. Symptoms can include memory loss, inability to communicate, confusion, disorientation, loss of logical thinking, etc. For vascular dementia, the lack of blood to the brain must be present over a long period of time, and the dementia will develop slowly.
Code 9310: Any dementia that does not have a known cause is rated under this code. All areas of mental functioning can be affected by dementia. Symptoms can include memory loss, inability to communicate, confusion, disorientation, loss of logical thinking, etc.
Code 9312: Dementia due to Alzheimer’s is a severe loss of mental ability because of the Alzheimer’s disease. All areas of mental functioning can be affected by dementia. Symptoms can include memory loss, inability to communicate, confusion, disorientation, loss of logical thinking, etc. In cases of Alzheimer’s, the dementia will usually grow gradually over time as the disease gets worse.
Code 9326: Dementia due to any other medical condition is a severe loss of mental ability because of another medical condition. Medical conditions that can cause dementia include endocrine system disorders, metabolic disorders, Pick’s disease, brain tumors, and more. Substance abuse, like drugs, alcohol, etc., can also cause dementia. All areas of mental functioning can be affected by dementia. Symptoms can include memory loss, inability to communicate, confusion, disorientation, loss of logical thinking, etc.
Code 9327: Organic mental disorders are any kind of decrease in brain function that is caused by a physical medical condition. Although seemingly the same, it is different than dementia. Dementia is an actual psychological illness, while an organic mental disorder is a decrease in mental function strictly caused by the actual brain being damaged by another physical condition.
Code 9400: Generalized anxiety disorder is severe, uncontrollable worry about day-to-day things. This worry is often irrational.
Code 9403: All phobias are rated under this code. Phobias are irrational, severe fears that are tied to specific things. Phobias can range from fear of things like spiders, strangers, blood, etc., to fear of situations like big crowds, flying, leaving the house without your pants on, etc. Phobias are more than just basic fear or dislike. They are often so severe that they lead to extreme behaviors like violence or panic attacks.
Code 9404: Obsessive-compulsive disorder is a condition where anxiety causes repetitive actions that are performed to reduce the fear. For example a person afraid of germs will wash their hands obsessively. Often the repetitive action is associated with numbers: washing their hands 14 (20, 5, whatever) times. These repetitive actions can interfere with the ability to work or perform daily tasks.
Code 9410: All other anxiety disorders are rated under this code.
Code 9411: Post-traumatic stress disorder is an anxiety condition that is caused by experiencing a traumatic event. A traumatic event can be defined as many different things, including car crashes, combat, death, abuse, extreme fear caused by an event, physical trauma, sexual abuse, or any other event that conflicts with an individual’s moral/natural ideals.
There are very explicit rules that must be followed in order to diagnose PTSD for Military Disability. The condition must fulfill all the following requirements in order to qualify for a PTSD rating.
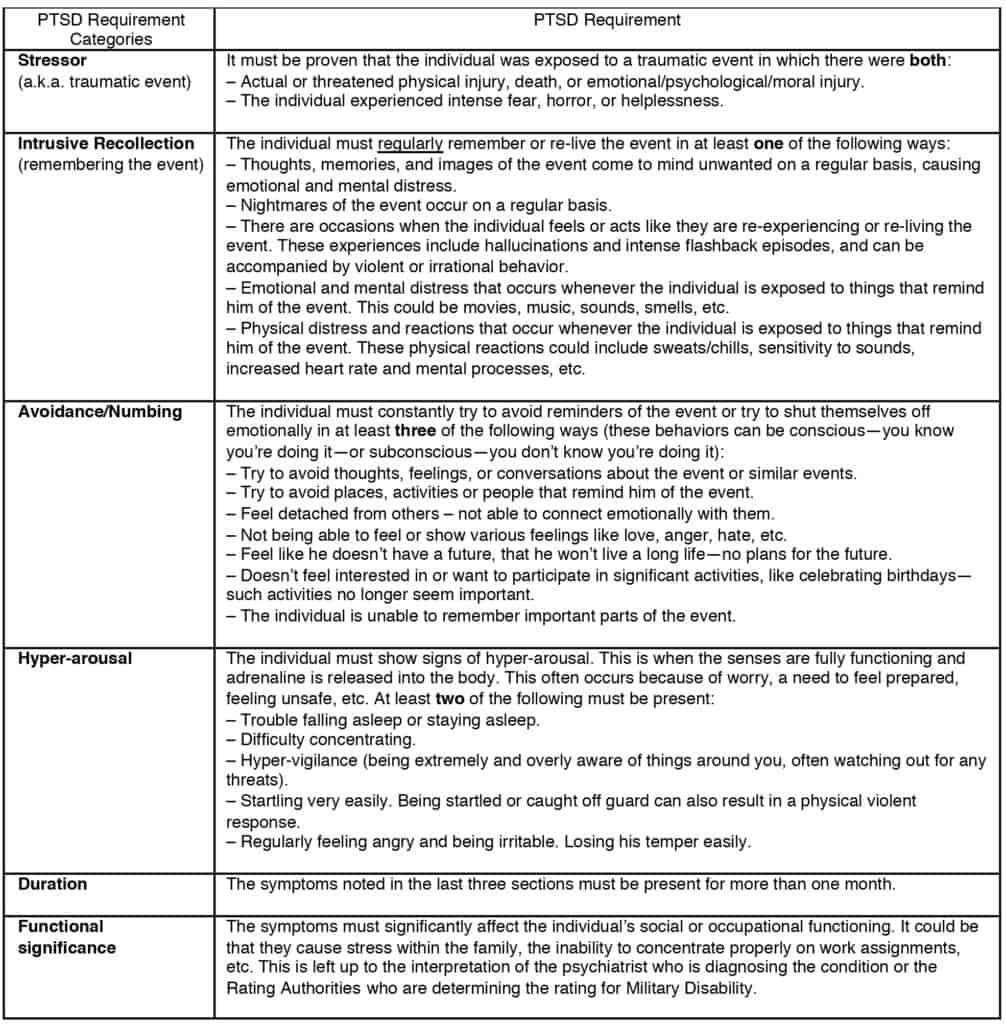
Code 9412: Panic disorder and/or agoraphobia are rated under this code. Panic disorder is a condition where severe panic attacks occur in stressful or fearful situations. Panic attacks are episodes of severe fear that causes the inability to act rationally. With panic disorder, the panic attacks can occur at any time and can last for a few minutes to many months. Agoraphobia is not the same as panic disorder, but often exists along with panic disorder. It is the fear of public places that can also cause panic attacks.
Code 9413: Other neuroses are rated under this code. A neurosis is an anxiety disorder that does not cause socially unacceptable behavior. This is a bit of a tough code to use since the next code (9410) is used for all other anxiety disorders that are not specifically noted elsewhere. So, which code would you use for an anxiety condition that has not yet been listed? If it does not cause socially unacceptable behavior (like violence or panic attacks), it can be rated under this code. All others are rated under code 9410.
Code 9416: Dissociative amnesia, fugue, and identity disorder (multiple personality disorder) are all rated under this code. Amnesia is the loss of memory, and can be long- or short-term memory. Fugue is basically amnesia that lasts for only a few hours up to a few days. Identity disorder is a condition where a person has at least 2 separate personalities that alternately control the person’s actions.
Code 9417: Depersonalization disorder is a condition where a person feels disconnected from their physical self. For example, they may feel like they are not in control of their body, that they are not a part of their body, that they are separated from their feelings and thoughts, that they cannot connect with their personality, that their reflection in a mirror is not actually them, etc. This condition is often the result of severe emotional and mental trauma.
Code 9421: Somatization disorder is a condition where the person regularly sees many different doctors complaining of pain, sexual problems, stomach problems, or nerve problems. These symptoms do actually exist in the patient, but there are no physical causes. The most common explanation, although not proven, is that the physical symptoms are the brain’s way of dealing with stress.
Code 9422: Pain disorder is a condition where the person feels intense pain in numerous locations in the body without a physical medical cause. The pain is real and can be debilitating.
Code 9423: Undifferentiated somatoform disorder includes all other somatoform disorders.
Code 9424: Conversion disorder is a condition where there are neurological symptoms without any neurological causes. Symptoms can include blindness, fits, numbness, paralysis and other nerve conditions.
Code 9425: Hypochondriasis disorder is a condition where a person (a hypochondriac) obsessively believes that they have a serious medical condition (often the believed medical condition changes regularly), but there is nothing at all wrong with their body.
Code 9431: Cyclothymic disorder (cyclothymia) is a condition where you alternate between very happy, euphoric moods and depression. It is like being bipolar, but the highs and lows are not as severe. There can also be periods of normal moods in between each high and low period.
Code 9432: Bipolar disorder is a condition where you fluctuate between extreme happiness (mania) and extreme depression. There is more to bipolarity than just mood, however. When experiencing mania, the entire body works harder and stronger. The brain speeds up and high energy levels are present. This can cause you to be radically impulsive and make bad decisions and behave inappropriately.
Code 9433: Dysthymic disorder (chronic depression) is a condition where there is depression that lasts a long time (at least 2 years), but is less severe than major depressive disorder.
Code 9434: Major depressive disorder (clinical depression) is a condition characterized by severe depression that causes low self-esteem, low energy levels, no motivation, no interest in social activities, etc.
Code 9435: All other mood disorders are rated under this code.
Code 9440: Chronic adjustment disorder is a condition that is caused by a particularly stressful period or event. Symptoms often include sadness, anxiety, hopelessness, anxiousness, trouble sleeping, etc.
March 9, 2012 – Primary Amyloidosis
Code 7717: Primary amyloidosis (a.k.a. AL amyloidosis, primary systemic amyloidosis, PSA, or amyloid light-chain amyloidosis) is a condition which causes the body to produce abnormal proteins that can build up and interfere with the functioning of the organs. It’s a bit of an odd condition since it’s not really a blood condition at all, but the VASRD stuck it in this category since there really wasn’t a better option. We don’t know what causes amyloidosis, and it can affect any organ or function in the body. There was no rating AT ALL for Amyloidosis before March 9, 2012. It had to be rated analogously (see the Analogous and Equivalent Codes page) with another condition.
January 19, 2012 – Amyotrophic Lateral Sclerosis (ALS)
Code 8017: Amyotrophic lateral sclerosis (a.k.a. Lou Gherig’s Disease or ALS) is a degenerative disease that gets worse over time and affects the nerve cells in the brain and spinal cord that control voluntary (you tell the muscle to move—as opposed to involuntary: the heart beats regardless of the brain) muscle movement. Symptoms include loss of coordination, weakness, difficulty eating (7203, 9901), breathing (6840-6841), nerve paralysis, double vision (6009), and weight loss.
This condition is rated on the same Central Nervous Rating System that we use currently, but the rating given for an ALS condition cannot be less than 30%.
December 10, 2008 – The Eyes
The majority of the eye rating system before 2008 was the same as the eye system we use today. There are a few important changes, though. The differences between the current VASRD and the one before 2008 are as follows:
The Visual Impairment Rating System
There are 3 different ways to evaluate vision problems: Visual Acuity, Visual Field, and Muscle Dysfunction. After the discussion of the rating system, we’ve included a list of all the eye conditions.
In the examinations, all the normal tests for rating visual acuity are required, but in addition, test results of the anatomy of the eye and any abnormalities should also be included.
Since visual acuity is rated on best corrected vision, glasses or contacts must be worn. Before 2008, however, only glasses could be worn, not contacts, unless the contacts were required for medical reasons.
In the current VASRD, there are a few special circumstances for rating visual acuity. Some of them were different before 2008 as follows:
- In a single eye, if there is a big difference between the near and far corrected vision, it is a special case that must be referred to the Director of Compensation and Pension Services for rating.
- If there are more than 4 diopters between the worse eye’s and the best eye’s prescription, the worse eye can be rated on uncorrected vision if it would give a higher rating than if it was rated on corrected vision.
The following is the chart of ratings for visual acuity. A few differences from the current one: The codes are listed below the ratings themselves since there were many more codes then than there are now.
“Light Perception Only” means that the eye cannot read the eye test chart 1 foot away from it and the eye is unable to see slight motion at 3 feet.
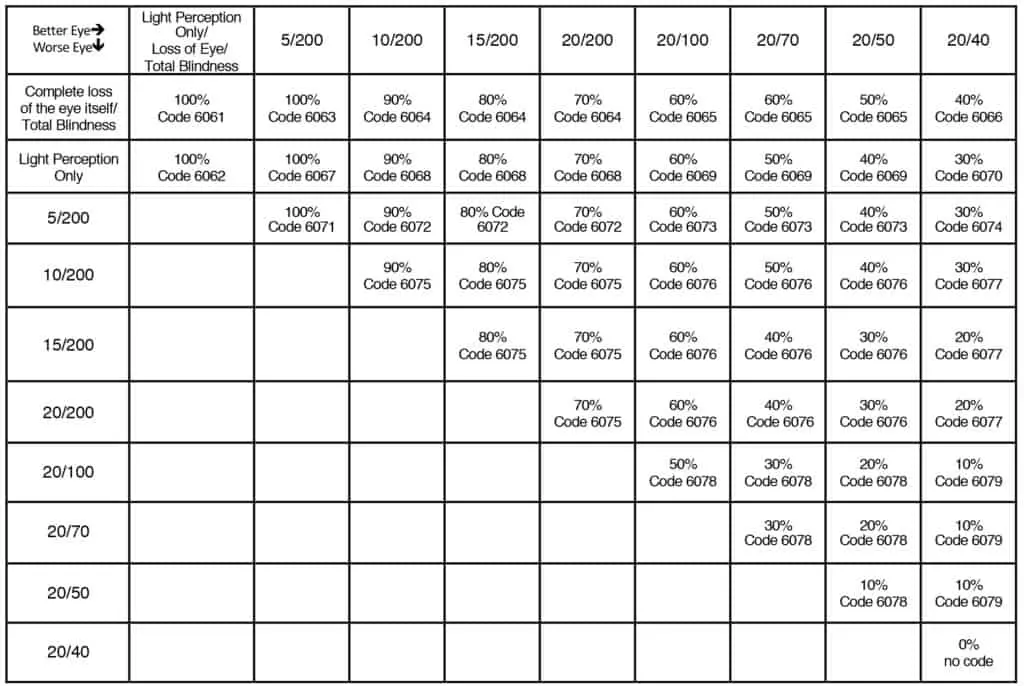
In the examinations, the visual field has to be tested using a standard perimeter and 3 mm white object. The test results should include a chart of the 16 meridians in each eye. This visual field must be performed at least twice, but three times is preferred. A tangent screen or campimeter test could be done in addition, but is not required.
The methods used to calculate the visual field are the same as the current VASRDs, but there are a few differences in the following code:
Code 6080: Impairment of the visual field. There are a number of things that rate under this code.
A 30% rating is given if one half of the visual field is lost in both eyes (“homonymous hemianopsia”).
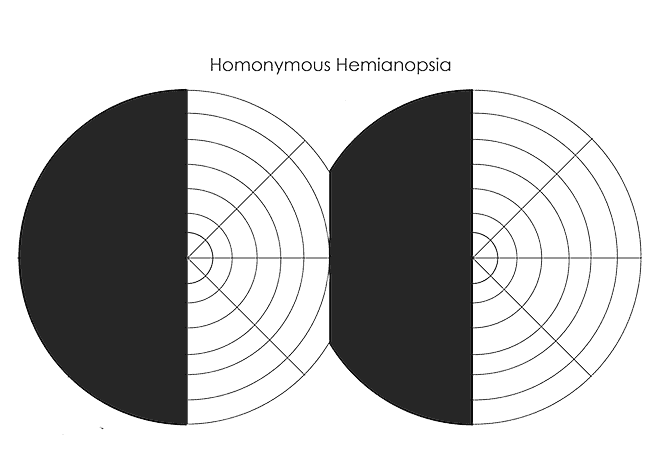
The temporal half of the visual field is the half that is away from the nose. If one eye is affected, it is rated 10%. If both eyes, 30%.
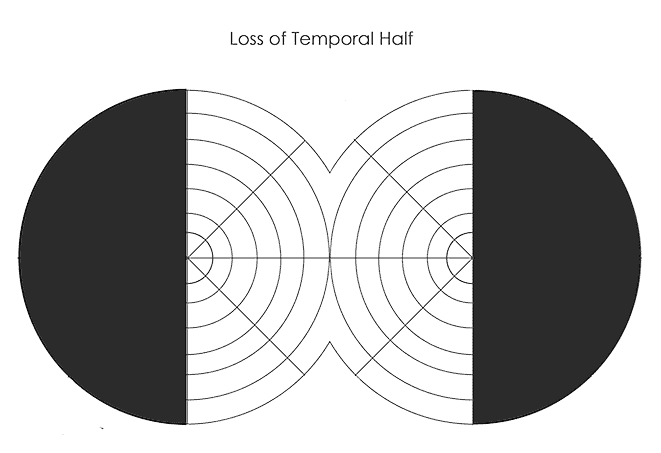
The nasal half is the part of the visual field towards the nose. If it is lost in one eye, it is rated 10%. In both eyes, 20%.
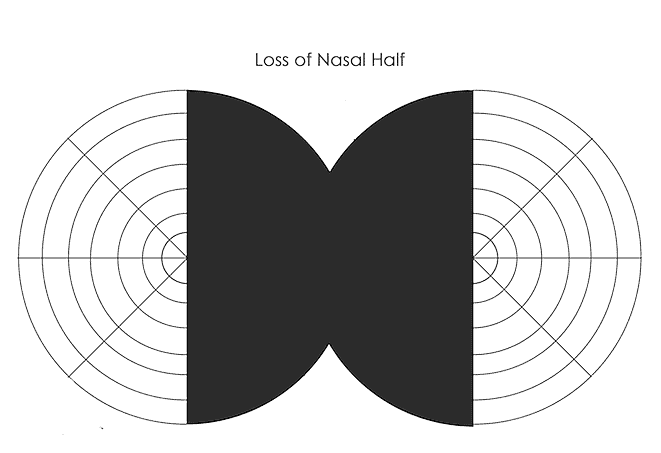
All other visual field contractions are rated as follows: If the field is contracted to 5° or less, it is rated 100% for both eyes and 30% for one eye. If it is contracted to between 6° and 15°, it is rated 70% for both eyes and 20% for one eye. If it is contracted to between 16° and 30°, it is rated 50% for both eyes and 10% for one eye. If it is contracted to between 31° and 45°, it is rated 30% for both eyes and 10% for one eye. If it is contracted to between 46° and 60°, it is rated 20% for both eyes and 10% for one eye.
Emphasis is put on the face that muscle dysfunction (also known as “diplopia”) must be directly diagnosed. Just occasional diplopia or correctable diplopia cannot be rated.
There are three codes that are used for rating muscle dysfunction before 2008:
Code 6090: Diplopia is a condition where the eye can look at one object and see two separate images.
Code 6091: Symblepharon is a condition where the outside of the eyeball adheres to the inside of the eyelid.
Code 6092: Diplopia due to limited muscle function. We don’t know why this is a separate code. Almost all diplopia is due to muscle dysfunction. That must be why they deleted this code in 2008.
All are rated according to the current Muscle Dysfunction Rating System. There is a change, however, when combining Muscle Dysfunction with Central Visual Acuity or Visual Field.
Muscle Dysfunction and Central Visual Acuity
Since there are two eyes, there are a few different possible combinations.
- If one eye has muscle dysfunction and the other has visual acuity, then just rate the one on muscle dysfunction and the other on its visual acuity.
- If both eyes have both muscle dysfunction and visual acuity, then rate the worst eye on muscle dysfunction, and the other on visual acuity.
- If one eye has muscle dysfunction and visual acuity, and the other only has visual acuity, rate the first on whichever would give the highest rating, muscle dysfunction or visual acuity.
That’s it. The current system that increases the visual acuity was not used before 2008.
Muscle Dysfunction and Visual Field
The changes for visual acuity are the same for visual field:
Since there are two eyes, there are a few different possible combinations.
- If one eye has muscle dysfunction and the other has visual field, then just rate the one on muscle dysfunction and the other on its visual field.
- If both eyes have both muscle dysfunction and visual field, then rate the worst eye on muscle dysfunction, and the other on visual field.
- If one eye has muscle dysfunction and visual field, and the other only has visual field, rate the first on whichever would give the highest rating, muscle dysfunction or visual field.
That’s it. The current system that increases the visual acuity after converting the visual field was not used before 2008.
Conditions of the Eye
Many of the eye conditions that were rated before 2008 are the same as the current VASRD, but there are still quite a few changes. To avoid confusion, all that were rated before 2008 are listed below. All the following conditions are rated on the Visual Impairment Rating System unless otherwise specified.
For codes 6000 – 6009, if the disease is active, then the minimum rating is 10%.
Code 6000: Uveitis is a condition where the uvea swells and becomes red.
Code 6001: Keratitis is the swelling of the cornea of the eye.
Code 6002: Scleritis is the swelling of the Sclera.
Code 6003: Iritis is the swelling of the iris.
Code 6004: Cyclitis is the swelling of the ciliary body, the muscles that help focus the lens.
Code 6005: Choroiditis is the swelling of the choroid, a thin layer of tissue below the sclera.
Code 6006: Retinitis is the swelling of the retina.
Code 6007: Intraocular hemorrhage is bleeding in the eye.
Code 6008: Detachment of the retina is a condition where fluid seeps under the retina and could lead to blindness.
Code 6009: Other eye injuries that are not healed are rated here.
Code 6010: Tuberculosis of the eye. This condition is rated as nonpulmonary tuberculosis.
Code 6011: Any condition or irregularity of the retina that is not covered elsewhere is rated here. It is rated 10% for one or both eyes.
Code 6012: Glaucoma (damage to the optic nerve) that is caused by swelling or by congestion is rated as Iritis, code 6003. If the condition has frequent, long attacks, then it is rated 100% while the attacks last.
Code 6013: Glaucoma (damage to the optic nerve) that is not caused by swelling or congestion is rated on the Visual Impairment Rating System. The minimum rating for this condition is 10%.
Code 6014: Malignant cancer in the eye is rated 100% while it is active. Once it is inactive, it is rated on the Visual Impairment Rating System.
Code 6015: Benign tumors in the eye are rated on the Visual Impairment Rating System. The minimum rating for an active tumor is 10%.
Code 6016: Central nystagmus is the twitching or excessive movement of the eye caused by a nerve condition. It is rated 10%.
Code 6017: Trachomatous conjunctivitis is a condition where a bacterial infection causes the conjunctiva to swell despite treatment. This condition is rated on the Visual Impairment Rating System. If the condition is active, the minimum rating is 30%.
Code 6018: All other Chronic conjunctivitis is rated 10% while it is active. If it is not active, it is rated 0%.
Code 6019: Ptosis is a condition where the eyelids droop. It is rated on the Visual Impairment Rating System. If the drooping eyelids completely block the pupil so that no vision is possible, it is given a visual acuity of 5/200. If more than half of the pupil is blocked, it is given a visual acuity of 20/100. If less than half is blocked, it is rated under code 7800, disfigurement.
Code 6020: Ectropion is a condition where weak muscles or tissue cause the lower lid to turn inside out. If both eyes have it, it is rated 20%. One eye is rated 10%.
Code 6021: Entropian occurs when an eyelid folds inward. If both eyes, it is rated 20%. One eye is rated 10%.
Code 6022: Lagophthalmos occurs when the eyelids can’t close completely. Two eyes is rated 20%, and one eye is rated 10%.
Code 6023: Complete loss of the eyebrows is rated 10%.
Code 6024: Complete loss of the eyelashes is rated 10%.
Code 6025: Any condition that hinders the production of tears is rated 20% if both eyes are affected, and 10% if one eye is affected.
Code 6026: Optic neuropathy occurs when the optic nerve is damaged. All conditions that damage the optic nerve that are not glaucoma are rated under this code. This condition can receive two different ratings: one under the Visual Impairment Rating System, and the other under the condition that causes the neuropathy.
Code 6027: A cataract is a condition where the lens in the eye becomes cloudy. It is rated under this code if it was caused by trauma. It is rated under the Visual Impairment Rating System. If surgery has been performed but no new lens implanted, it can also be rated as aphakia (below).
Code 6028: If the cataract was not caused by trauma, it is rated under this code. It is rated under the Visual Impairment Rating System. If surgery has been performed without a new lens implanted, it can also be rated as aphakia (below).
Code 6029: Aphakia is the absence of a lens in the eye.
There are two different ways aphakia can be rated. It can be rated 30% if one or both eyes are aphakic, or it can be rated on the Visual Impairment Rating System, whichever gives the higher rating. Just one or the other, never both.
If using the Visual Impairment Rating System:
If one eye has aphakia and the other has visual acuity, then the eye with the visual acuity can be rated on its uncorrected acuity.
If both eyes have aphakia, both are rated on their corrected visual acuity, BUT neither can be assigned a visual acuity better than 20/70. So if both eyes are 20/50, then both would be moved down to 20/70 for rating. If both are already 20/70 or worse, then one of them is moved down to the next worse acuity. So, if the corrected acuity of the right eye is 20/70, and the other is 20/100, then one of them can move down to the next worse. Choose the one that would give the best rating. In this example, 20/100 could move to 20/200, but the rating for 20/70 and 20/200 is only 40% while the rating for 20/100 and 20/100 is 60%.
Code 6030: Paralysis of accommodation occurs when the Oculomotor Nerve is damaged. It is rated 20%.
Code 6031: Dacryocystitis is the welling of the nasolacrimal sac which produces tears. It is rated as production of the tears.
Code 6032: If part or all of the eyelids are missing, it is rated as disfigurement, code 7800.
Code 6033: The dislocation of the crystalline lens is rated as aphakia (above).
Code 6034: Pterygium occurs when conjunctiva fibers grow into the cornea. It is rated on the Visual Impairment Rating System.
Code 6035: Keratoconus occurs when the cornea slowly changes shape over time. It is rated on the Visual Impairment Rating System on the corrected vision wearing contact lenses. If the contacts are medically required, the minimum rating is 30% for one or both eyes.
October 23, 2008 – Traumatic Brain Injury (TBI)
Before 2008, rating traumatic brain injury (TBI) was a lot more simple than it is now. It was referred to as brain disease due to trauma, and was rated as follows:
Code 8045: Brain disease due to trauma is a condition of the brain that occurs after it receives a traumatic injury, like hitting your head in a car accident, or having shrapnel pierce through your skull into the brain.
If there are any serious symptoms like seizures, paralysis, mental disorders, etc., then each symptom is rated on its own. So, seizures would be rated as epilepsy, paralysis would be rated on the affected nerve, etc. All of these conditions must be distinctly diagnosed in order to be rated. (The ratings for the majority of these conditions are the same in 2008 as they are now, but double check this page before proceeding to the current ratings just to make sure).
If there are only symptoms that are not conditions in and of themselves (like headaches, dizziness, insomnia, etc.), then they are all rated together for one single rating of 10% under code 9304, dementia due to trauma. For a higher rating than 10% under this code, dementia itself would have to be clearly diagnosed.
The final rating for any these conditions will look like this: 8045-8910. The first four-digit code defines head trauma as the cause of the condition, and the second four-digit code tells what symptom is being rated, in this case epilepsy (8910).
October 23, 2008 – The Skin
The Skin ratings changed twice since 2001, once in 2002 and once in 2008. Many of the skin codes are exactly as they are now, and so will not be discussed here. The differences are as follows:
Code 7801: Scars on the body (not the head, face, or neck) that are either deep or limit the motion of the affected body part. This condition is rated on the amount of skin that is affected by the scar. The areas of the scar do not have to be attached to contribute to this rating, but if they are clearly and significantly separate, then they are rated separately. For example, if there are numerous patches of scars on the torso, then they would all contribute to a single rating since they are pretty much the same. If, however, there were patches of scars on both arms, they would be rated separately since they are clearly different.
If the scars cover 144 in2 or more, it is rated 40%. If they cover 72 in2 or more, it is rated 30%. 12 in2 or more is rated 20%, and 6 in2 or more is rated 10%.
Code 7802: Scars on the body (not the head, face, or neck) that are not deep and do not limit the motion of the affected body part. This condition is rated on the amount of skin that is affected by the scar. The areas of the scar do not have to be attached to contribute to this rating, but if they are clearly and significantly separate, then they are rated separately. For example, if there are numerous patches of scars on the torso, then they would all contribute to a single rating since they are pretty much the same. If, however, there were patches of scars on both arms, they would be rated separately since they are clearly different.
If the scars cover 144 in2 or more, it is rated 10%.
Code 7803: Any scar that is Superficial and frequently loses the skin over the scar is rated 10%.
Code 7804: Any scar that is Superficial and painful to the touch is rated 10%.
Code 7805: All other scars are rated on the body part that it affects. So, if a scar on the elbow keeps the elbow from bending all the way, then it would be rated on limited motion of the elbow.
October 6, 2006 – The Respiratory System and The Cardiovascular System
The rating systems for the Respiratory and Cardiovascular Systems are exactly the same, but before 2006, there were a few tests that were not required that are now required. These tests include:
For the Cardiovascular System:
- MET Tests
For the Respiratory System:
- Pulmonary Function Tests
- DLCO (SB)
- Post-bronchodilator studies
These tests do factor into the ratings before 2006, but there were no rules regarding having to have them done and how exactly to use the test’s results. Basically all Respiratory and Cardiovascular conditions were rated exactly as they are now, but with a little more room for the Rating Authorities to decide how best to use the test results to rate the condition. You can pretty much ignore this, really.
September 26, 2003 – The Spine
A big change was applied to the VASRD in 2003 updating all the Spine ratings and changing the code numbers to what they are now. Before 2003, all spine conditions were rated as follows:
Code 5285 (changed to code 5235): Vertebral fracture occurs when the bones in the spine break. This can occur anywhere along the spine, and so can cause many different symptoms.
If this condition damages the spinal cord, requires the use of long leg braces, or makes the service member bedridden, it is rated 100%. If the condition does not damage the spinal cord, but requires the use of a neck brace, it is rated 60%.
All other vertebral fracture conditions are rated on limited motion of the spine (codes 5286–5292, below). When choosing the code for limited motion, there are three sections of the spine to consider: cervical, dorsal, and lumbar. If one is definitely disabled, but the others only have minor involvement, then only the one can be rated. If, however, each segment is significantly affected, then each can be rated separately.
Code 5286 (changed to 5240 and 5241): Complete bony fixation of the spine occurs when the spine fuses together (either on its own or surgically), and cannot move at all. If the spine is stuck in an unnatural position (like curving drastically or leaning to the side), it is rated 100%. If it is frozen in a normal spine shape, it is rated 60%.
Code 5287: If the Cervical Spine cannot move at all, it is rated 40% if it is frozen in an unnatural position and 30% if it is frozen in the normal spine position. (This code was deleted completely when the spine rules changed.)
Code 5288: If the Dorsal Spine cannot move at all, it is rated 30% if it is frozen in an unnatural position and 20% if it is frozen in the normal spine position. (Deleted.)
Code 5289: If the Lumbar Spine cannot move at all, it is rated 50% if it is frozen in an unnatural position and 40% if it is frozen in the normal spine position. (Deleted.)
Code 5290: If the Cervical Spine is limited in motion, it is rated 30% if it cannot move much at all. If it can move some, but is still pretty limited (maybe cannot turn the head all the way to either side, etc.), it is rated 20%. If it is limited in motion, but can overall still move the head without much difficulty, it is rated 10%. (Deleted.)
Code 5291: If the Dorsal Spine is limited in motion, it is rated 10% if it is definitely limits its ability to function. If it is limited, but can overall still function without much difficulty, it is rated 0%. (Deleted.)
Code 5292: If the Lumbar Spine is limited in motion, it is rated 40% if it can hardly move at all. If it can move some, but is still pretty limited (maybe cannot bend more than 45° forward, etc.), it is rated 20%. If it is limited in motion, but can overall still bend over most of the way without much difficulty, it is rated 10%. (Deleted.)
Code 5293 (changed to code 5243): Intervertebral Disc Syndrome occurs when a disc in the spine is dysfunctional. It can deteriorate, herniate, etc. It is rated one of two ways. The first is on Incapacitating Episodes, which is the same as it is now. It can also be rated as follows:
Since intervertebral disc syndrome can affect any part of the spine, it can cause many different symptoms, like nerve pain, limited motion, etc. Any of these symptoms that is always present and distinct from the other symptoms can be separately rated. All these ratings are then combined using VA Math to get one overall rating for this condition.
This overall rating can be used to rate the condition or the rating for Incapacitating Episodes, whichever is higher.
The following two codes are rated the same:
Code 5294 (changed to 5236): Sacroiliac injury and weakness is any injury or condition of the Sacroiliac Joint.
Code 5295 (changed to 5237): Lumbosacral strain is any pain or injury to the low back and lumbosacral joint.
These codes are both rated as follows:
A 40% rating is given if there is limited motion with severe symptoms like the inability to bend forward very far, the spine leans abnormally off to the side, the affected joint is irregular or narrowed, or the inability for the torso to bend to the sides and there is confirmed arthritis is the affected joint.
A rating of 20% is given if there are muscles spasms when bending very far forward, or if the torso cannot bend to the sides at all when standing.
A 10% rating is given if there is pain with motion.
All other minor symptoms are rated 0%.
That’s all the old spine codes. All other spine conditions are rated analogously (see the Analogous and Equivalent Codes page) with these codes.
July 1, 2003 – Liver Abscess
On July 1, 2003, the code 7313 for abscess of the liver was removed. Liver abscesses are normally caused by another condition, and so should not be separately rated. Just rate the condition that causes it. Before this date, however, they could be rated as follows:
Code 7313: A liver abscess is a pocket of pus inside the liver. If it causes serious symptoms like extreme pain, or interferes seriously with the liver’s ability to function, it is rated 30%. If the symptoms are moderate (they are definitely there and limit the body’s overall functioning, but not seriously), it is rated 20%.
June 13, 2003 – Tinnitus
Code 6260: Tinnitus is ringing in the ears that often occurs after exposure to serious aural trauma like explosions. It has always been rated 10%, but before this date, there were less rules about how to rate it.
Now, only one rating for tinnitus can be given whether or not it is in only one or both ears. It is safe to assume that this was standard practice even before 2003, but it now clearly states it. It also states now that tinnitus cannot be rated if it is definitely caused by another condition, like a mental disorder or another physical disorder. Again, this was probably common practice since a single symptom cannot be rated twice, but the VASRD just got more specific on it after June 13, 2003.
September 23, 2002 – Intervertebral Disc Syndrome
Before this date, intervertebral disc syndrome was rated as follows:
Code 5293 (changed to code 5243): Intervertebral disc syndrome occurs when a disc in the spine is dysfunctional. It can deteriorate, herniate, etc.
If the condition causes constant, significant symptoms like pain down the arms or legs, muscle spasms, loss of nerve reflexes, etc., it is rated 60%. If the symptoms are severe, but not constant, it is rate 40%. If the symptoms are not severe but still fairly significant, regardless of whether or not they are constant, it is rated 20%. Mild symptoms are rated 10%. If there are no symptoms or if surgery was successful in eliminating the symptoms, it is rated 0%.
August 30, 2002 – The Skin
Note: The skin ratings change twice. Once 2002 and once again in 2008.
Before 2002, the skin ratings had room for quite a lot of interpretation. When they changed, they became more based on measurable facts instead of just personal opinion. The skin was rated as follows:
Code 7800: Scars of the head, face, or neck. If the scars are extremely serious, causing the head, face, or neck to be repulsive on one side of the face, or if the scars are a bit less repulsive but affect both sides of the face, it is rated 50%. If the scars are severe, and cause an obvious deformity of the eyelids, lips, or ears, it is rated 30%. If the scars are clearly present, but not seriously repulsive, with little or mild deformity, it is rated 10%. All lesser scars are rated 0%.
In addition to these ratings, if the scars are also dramatically discoloured (i.e. dark, white, red, etc.), they increase the above ratings. 50% becomes 80%, 30% becomes 50%, and 10% becomes 30%. 0% is not increased.
Code 7801: Third degree burn scars. Third degree burns affect all three layers of the skin. This condition is rated on the amount of skin that is affected by the burn scar. The areas of the burn scar do not have to be attached to contribute to this rating, but if they are clearly and significantly separate, then they are rated separately. For example, if there are numerous patches of scars on the torso, then they would all contribute to a single rating since they are pretty much the same. If, however, there were patches of scars on both arms, they would be rated separately since they are clearly different.
If the burn scars cover 144 in2 or more, it is rated 40%. If they cover 72 in2 or more, it is rated 30%. 12 in2 or more is rated 20%, and 6 in2 or more is rated 10%.
Code 7802: Second degree burn scars. Second degree burns affect the first two layers of skin. This condition is rated on the amount of skin that is affected by the burn scar. The areas of the burn scar do not have to be attached to contribute to this rating, but if they are clearly and significantly separate, then they are rated separately. For example, if there are numerous patches of scars on the torso, then they would all contribute to a single rating since they are pretty much the same. If, however, there were patches of scars on both arms, they would be rated separately since they are clearly different. If the burn scars cover 144 in2 or more, it is rated 10%.
Code 7803: Superficial scars with regular ulcerations. If the scar often has an open wound with infection, it is rated 10%.
Code 7804: Superficial scars that are tender to the touch are rated 10%.
Code 7805: All other scars are rated on the body part they affect. For example, there is a scar over the elbow that limits the elbow’s ability to bend all the way, it would be rated on limited motion of the elbow.
Code 7806: Eczema or dermatitis is the irritation of the skin—the basic rash. If the rash is extremely severe and repulsive, with the skin constantly peeling or crusting or causing open, infected wounds, it is rated 50%. If the rash is constantly oozing, constantly itchy, causes open wounds (not infected necessarily), or is disfiguring, it is rated 30%. If the rash is on a part of the body that is visible (the head, neck, and hands) or covers a lot of the body, and has any peeling, oozing, or itchiness, it is rated 10%. If the rash is small and not on a visible part of the body, and has any peeling, oozing, or itchiness, it is rated 0%.
Code 7807: American (“New World”) leishmaniasis is a parasitic infection on the skin caused by an American sandfly bite. This condition is rated as eczema, code 7806.
Code 7808: Old World cutaneous leishmaniasis (“oriental sore”) is a parasitic infection on the skin caused by the bite of an Asian, African, or European sandfly. This condition is rated as eczema, code 7806.
Code 7809: Lupus that affects the skin is a condition where the healthy cells of the skin are attacked by the immune system. This condition is rated as eczema, code 7806.
Code 7810: Pinta is a skin infection most often found in Central and South America. This condition is rated as eczema, code 7806.
Code 7811: Tuberculosis luposa is lupus caused by tuberculosis. While it is active, it is rated 100%. Once it is not active, it is rated on the current rating schedule for nonpulmonary tuberculosis.
Code 7812: Verruga Peruana is a condition where warts form because of a bacterial infection. This condition is rated as eczema, code 7806.
Code 7813: Ringworm (“dermatophytosis”) is a red rash that is shaped like a ring. It is caused by a fungal infection. This condition is rated as eczema, code 7806.
Code 7814: Tinae barbae is a fungal infection of the hair. This condition is rated as eczema, code 7806.
Code 7815: Pemphigus is a bullous disorder that causes pockets (blisters) of clear fluid to form between layers of skin. This condition is rated as eczema, code 7806.
Code 7816: Psoriasis is a condition where the body produces too many skin cells because of an autoimmune disorder. This condition is rated as eczema, code 7806.
Code 7817: Dermatitis exfoliative is dermatitis (a rash) that covers the entire body. This condition is rated as eczema, code 7806.
Code 7818: Malignant skin cancer is rated under the skin code that best describes them. So, if it causes disfigurement of the face, it is rated under code 7800, etc.
Code 7819: Other skin growths (non-cancerous) are rated under the skin code that best describes them. So again, if it causes disfigurement of the face, it is rated under code 7800, etc.
August 26, 2002 – The Fingers
Quite a few changes happened for finger ratings in 2002, although the majority of the ratings are the same. It’s difficult to detail the changes, so instead we’ve just noted the complete rating system for these conditions. These changes are only for frozen joints and joints with limited motion. All amputation and other finger ratings are the same as they are now.
Note: Ratings for hand conditions often have different ratings for the dominant and non-dominant hands. “Dominant” refers to the hand you use to write, i.e. right-handed or left-handed. This means that the non-dominant hand is your other hand. If you happen to be ambidextrous, then whichever hand is affected by the condition is considered the dominant hand.
Double Note: If you have multiple different kinds of problems with the fingers on the same hand, then the hand is only given one rating for all of these problems together. For example, if your right hand has the pinky amputated, the ring finger frozen so that it cannot move, and the middle finger can move but only a little bit, then you’d only get one rating for all of these conditions. Rate the entire hand under the type of condition that best describes the overall hand disability. So, if you have two fingers frozen and one amputated, then rate all three fingers as though they were frozen since that is the majority condition.
Final Note: Rate each hand separately. While all the fingers on one hand only receive one rating all together, each hand can receive its own rating. So, if you have a frozen finger on the right hand and two on the left, then the right hand would get a rating for the one, and the left would get another rating for the two.
A condition will be rated here if one or more finger joints are frozen in place and cannot move at all or if they have limited motion. All ratings for frozen finger joints limited motion are based on “favorable” and “unfavorable” positions. The image below shows the different Finger Joint groups. These groups come into play when defining “favorable” and “unfavorable.”
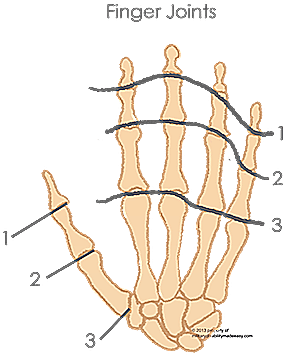
Favorable position:
Frozen Joints: The finger joint(s) are frozen bent so that the fingertip(s) are within 2 inches of the transverse crease. In other words, there is not more than 2” between the palm and tips of the finger(s).
Limited Motion: The finger joints are cannot bend the finger to touch the transverse crease completely, but are able to bend the finger to within 2 inches of the palm. In other words, the fingertip can bend so that there is less than 2 inches between it and the palm.
Unfavorable position:
Frozen Joints: Two different things qualify as unfavorable: (1) The finger joint(s) are frozen with more than 2” between the transverse crease and the tip of the finger. (2) Both Joints 2 and 3 (see the Finger Joints image above) are frozen on a single finger, even if they are frozen in a favorable position.
Limited Motion: The finger joint is not able to bend the finger to less than 2 inches away from the transverse crease. In other words, there is always more than 2 inches between the fingertip and the palm.
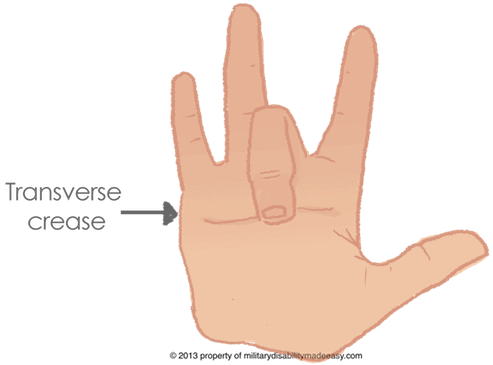
Extremely unfavorable position:
Frozen Joints: If only 1 finger is affected: All the finger joints are frozen so that the finger is completely straight, the finger joints are all frozen so that the finger is completely closed (like making a fist, but with just one finger), or the joints are frozen so that the bones of the finger do not align as they should, but twist or angle off to the sides.
If multiple fingers are affected: Both Joints 2 and 3 (see the Finger Joints image above) are frozen on each affected finger (or the majority of affected fingers), AND at least one of these joints on each finger is either frozen completely straight or completely bent.
Limited Motion: None.
One Finger
Two Fingers
Three Fingers
Four Fingers
Five Fingers
One Finger
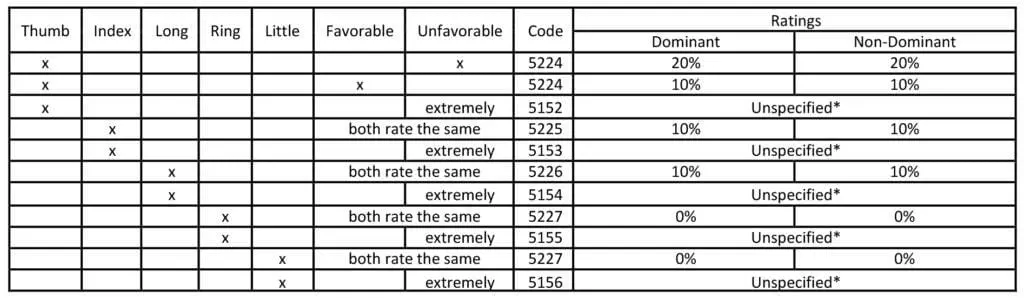
*This old VASRD does not specify the degree of amputation to rate under. See the Single Finger Amputations chart and rate the condition on the closest amputation option.
Return to Top Return to Fingers
Two Fingers
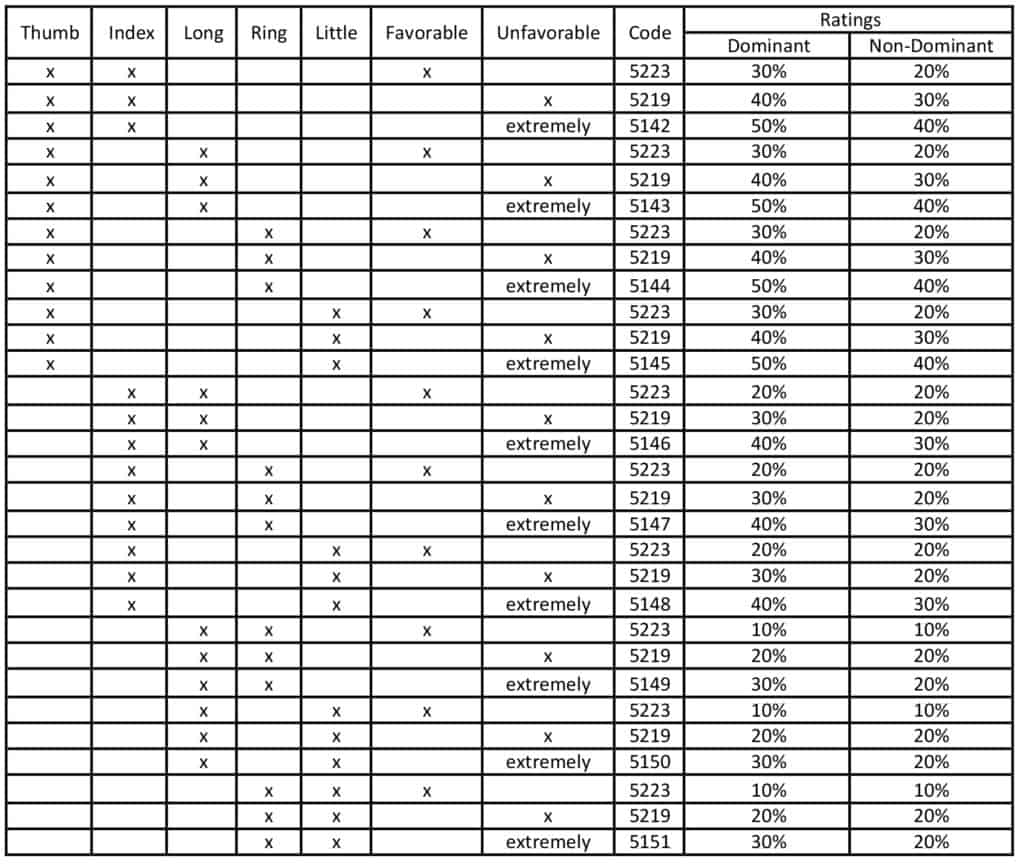
Return to Top Return to Fingers
Three Fingers
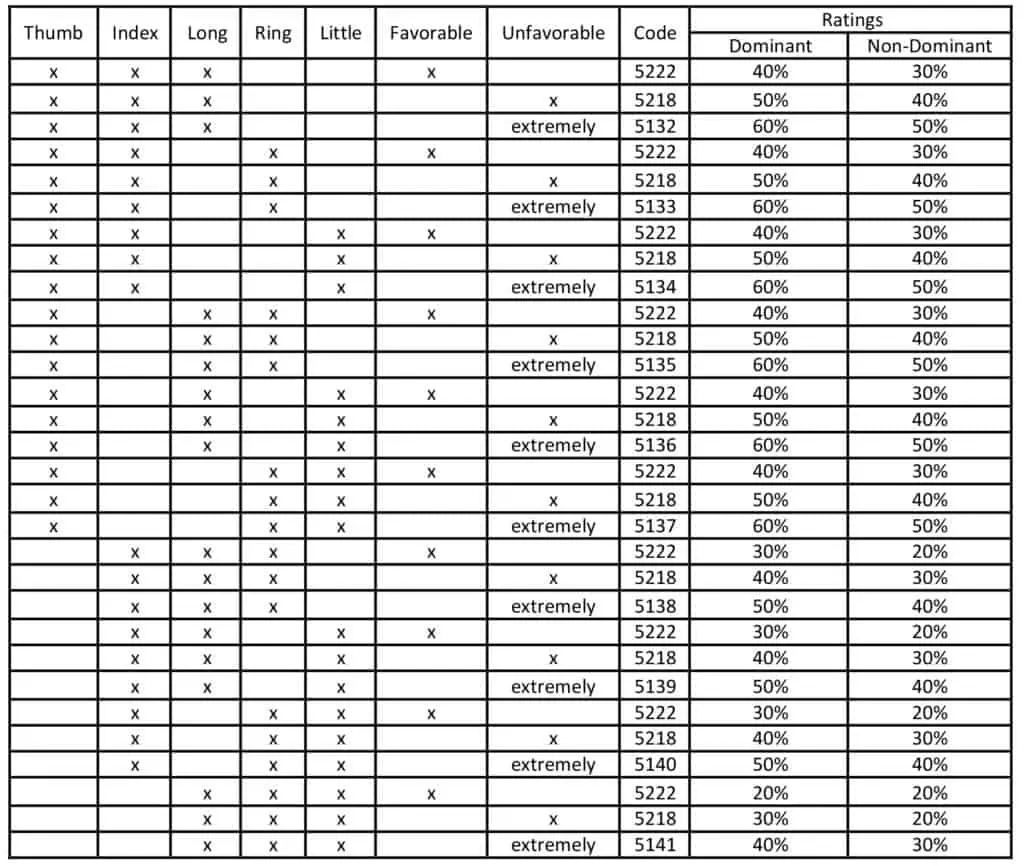
Return to Top Return to Fingers
Four Fingers
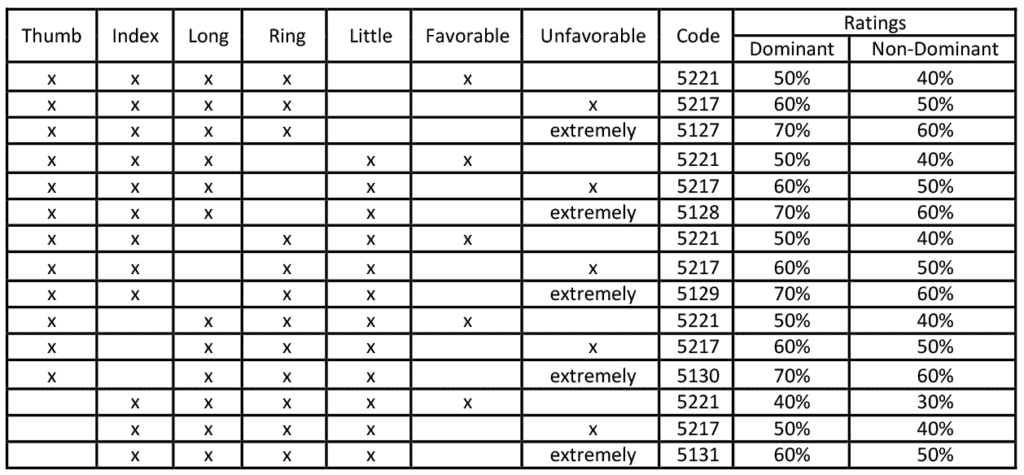
Return to Top Return to Fingers
Five Fingers
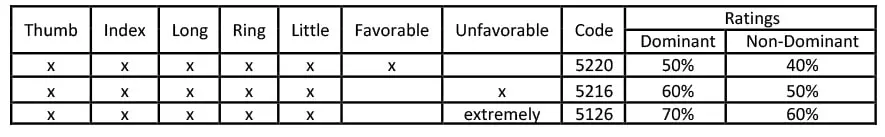
March 18, 2002 – The Removal of the Breast
Before this date, Special Monthly Compensation was not given for the removal of the breasts under Category K.
That’s it. If you were separated between 2001 and today, and you did not find your condition on this page, you can Find Your Condition on our site. It will be rated exactly as it is now, so you don’t have to worry about it.
FAQ's
What are historic VASRDs?
Historic VASRDs are previous versions of the Veterans Affairs Schedule for Rating Disabilities (VASRD).
Are historic VASRDs still used?
Yes. The VA uses the historic VASRDs to determine appeals of decisions made during an earlier version of the VASRD. Appeal decisions are based on the rating requirements at the time of the original decision/effective date, not the current VASRD.
If I submit my claim on the effective date of a change, will it be rated on the historic VASRD requirements or current requirements?
It depends on the official ruling for the change, but in most cases, anything submitted on or after the effective date are rated only on the new requirements.
Can I request to be rated on a historic VASRD?
No. There are strict rules in place for applying the VASRD. If you apply after a change has been made, you cannot be eligible for earlier rating options.
I have a condition currently rated but it will rate higher under the new coming changes. Will my rating increase?
In most cases, the VA will not update ratings already in effect when a change is made. However, there have been some rulings that clearly state that all current ratings will be automatically updated to the new ratings. This is rare. Usually, the only way to be rated on the new requirements would be to apply for an increased evaluation.
Why does the VASRD change?
The VA and Congress will update the VASRD occasionally over time in order to make the ratings more accurate, fair, and aligned with modern medicine.
Does the DoD use the historic VASRDs?
Yes, since 2008, the DoD has used the VASRD as their rating standard and so all VASRDs since then are applicable to the DoD. When the change was made in 2008, the PDBR was also formed to review veterans' cases from 2001 to 2008 and update their ratings to the historic VASRD in effect at the time of their separation.





